Tired of guessing which vitamins and nutrients you need more of? Use your genetic raw data from 23andMe or AncestryDNA to find out!
Here are five examples of how you can use your genetic data to understand how your genes can influence your need for specific nutrients. This is a great starting point for learning more about how your genes interact with your diet and your lifestyle.
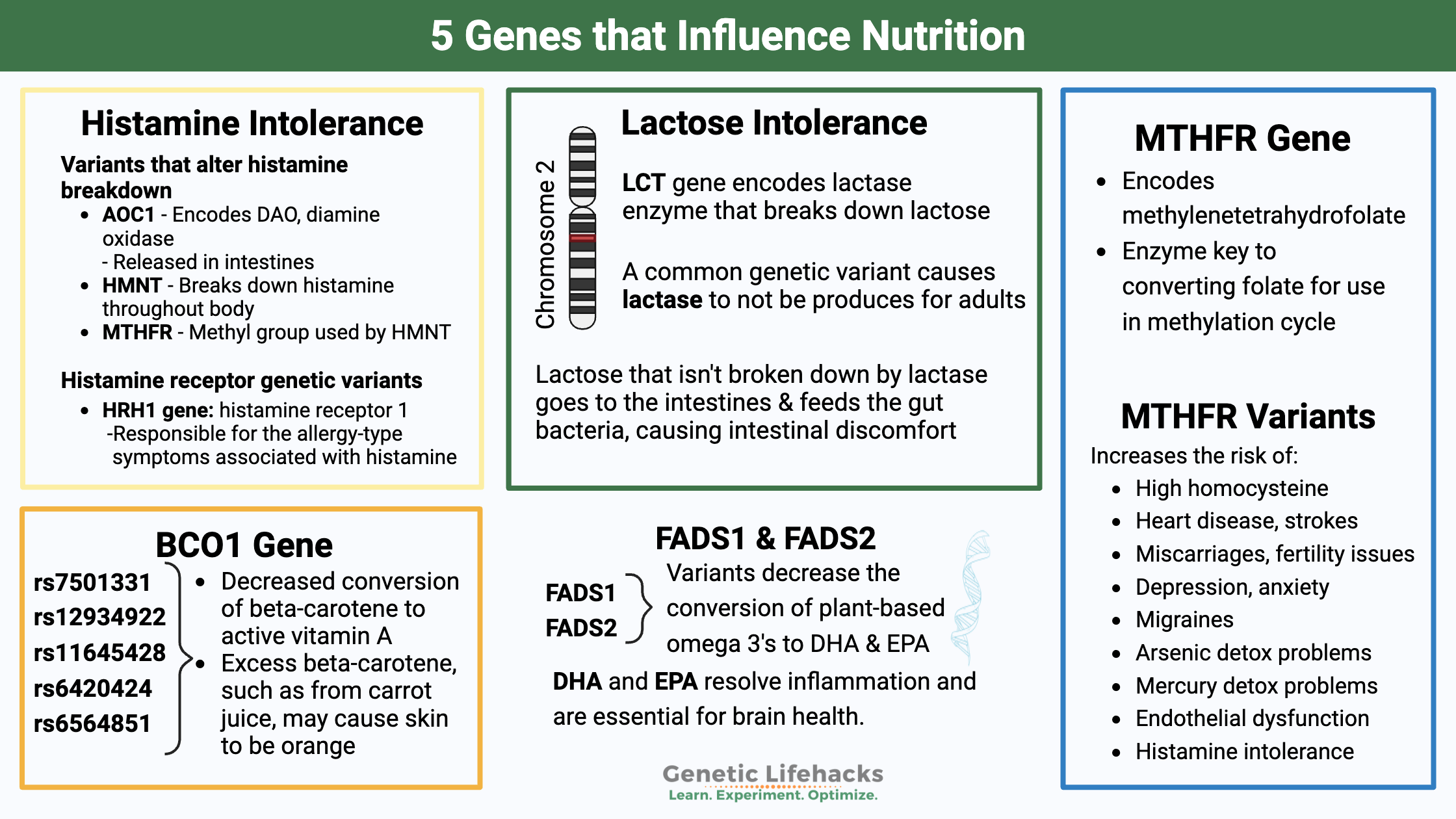
1. Vitamin A (BCO1 gene)
Vitamin A is a general term that covers several different forms of the vitamin.
- Animal food sources mainly provide retinyl palmitate, which breaks down in the intestines into retinol. It is stored, in this form, by the body and then converted to an active form for use.
- Carotenes are the plant forms of a precursor to vitamin A. The most common form, beta-carotene, shows up in abundance in carrots and other orange-colored foods. An enzyme in the intestine breaks down beta-carotene, converting it into retinol.[ref]
The cells in your body use retinoids in a variety of ways.
Retinol is important for:
- Stem cells
- Photoreceptors in the eye
- Epithelial cells
- Embryonic cells
- Various immune cells
- Red blood cells
- Circadian rhythm
Once beta-carotene has been digested, mixed with fats, and absorbed, it has to be converted into retinol. The BCO1 gene converts beta-carotene into retinal. The retinal converts into retinol.[ref]
Genetic variants in the BCO1 gene cause varying amounts of the enzyme to be produced and cause a large difference in the amount of vitamin A produced from dietary beta-carotene.
There is also a feedback loop in the body where higher levels of retinoic acid will decrease the production of the BCO1 enzyme, thus decreasing the amount of beta-carotene converted to retinal.[ref]
The BCO1 enzyme is active in the intestines, liver, and mucosal epithelium (e.g., lining of the lungs). As a result, the conversion of beta-carotene to vitamin A occurs in all of those locations.[ref]
Deficiency: A deficiency in vitamin A can cause poor night vision, worsen infectious diseases, and, when severe, cause blindness. In the immune system, retinol is involved with both innate and adaptive immune responses.[ref]
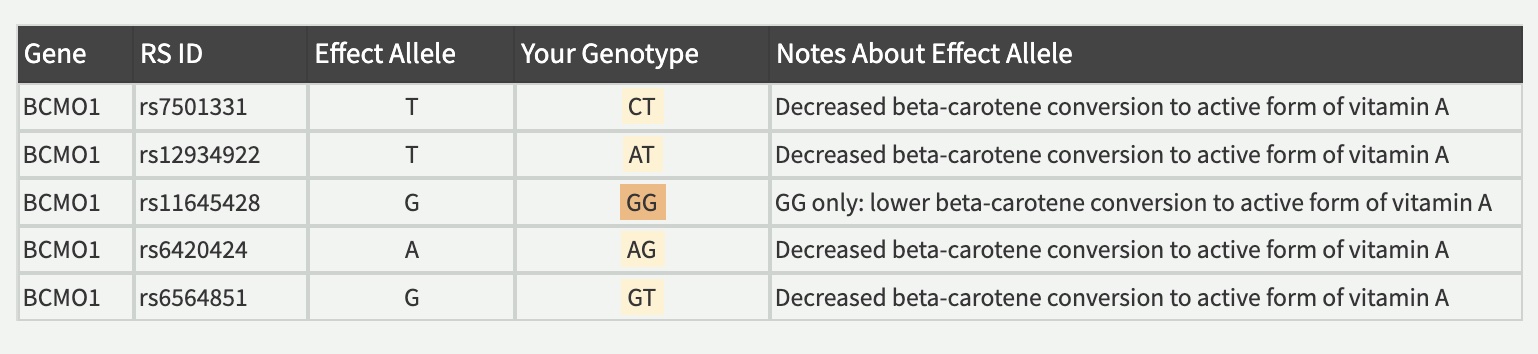
Here’s a sample of what you will see about your genes as a member:
Lifehacks:
If you have genetic variants related to converting beta-carotene to active vitamin A, there are several ways to boost your active vitamin A:
- eat foods rich in active vitamin A, such as liver, dairy, or pasture-raised eggs
- supplement with the retinyl palmitate form of vitamin A to increase your levels short-term
Caution with high-dose vitamin A:
Vitamin A is a fat-soluble vitamin that can build up in the body, so you don’t want to go overboard with it. (Get a blood test to determine your level.)
☑ Include vitamin D with vitamin A:
Studies show that too much vitamin A without enough vitamin D can be a risk factor for osteoporosis.[ref]. If you aren’t supplementing with vitamin D, make sun exposure each day a priority. Also, if you check your vitamin A levels, make sure you test your vitamin D levels at the same time.
☑ Include fat with beta-carotene for absorption: Beta-carotene is hydrophobic and needs fat to be absorbed in the intestines. Adding a little fat to your beta-carotene-rich food should help a little with absorption.[ref]
Ideas for better beta-carotene absorption:
- include butter or coconut oil with your vegetables
- add an avocado to your carrot-rich smoothie
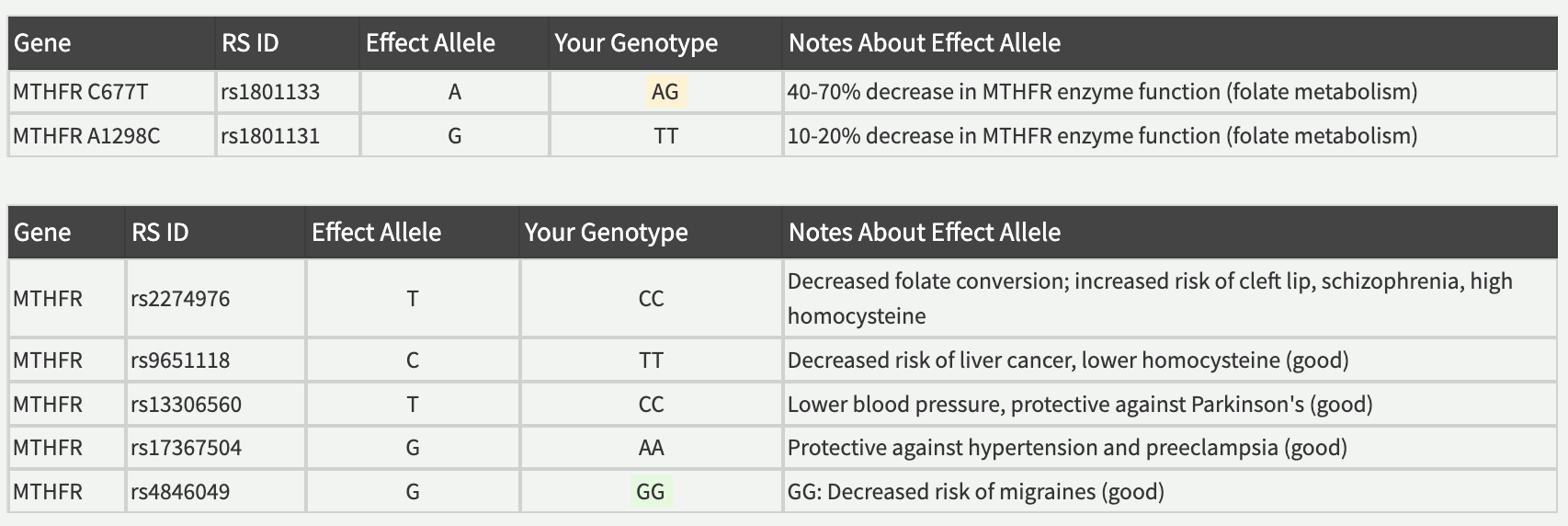
2. Folate (MTHFR gene)
MTHFR is a central gene in the methylation cycle and is a limiting factor for producing methyl groups from folate (vitamin B9). Common genetic variants, called MTHFR C677T and A1298C, affect how the enzyme works and impact the availability of methyl groups.
Methylation is the addition and removal of a methyl group (-CH3) to amino acids, DNA, and other enzymes or proteins. Within the methylation cycle, folate can be used to donate a methyl group that is used by SAMe for methylation reactions.
Methyl groups are used to:
- Form new molecules, including neurotransmitters
- Control DNA gene expression (turn on and off genes)
- Detoxify certain substances
Studies show that the C667T and A1298C variants increase the risk of numerous health conditions:
- high homocysteine levels, stroke risk, and heart disease[ref][ref][ref]
- neural tube defects (spina bifida) and cleft lip[ref]
- stroke[ref][ref]
- preeclampsia and hypertension in pregnancy[ref][ref]
- miscarriage[ref][ref]
- depression or anxiety[ref][ref][ref][ref][ref]
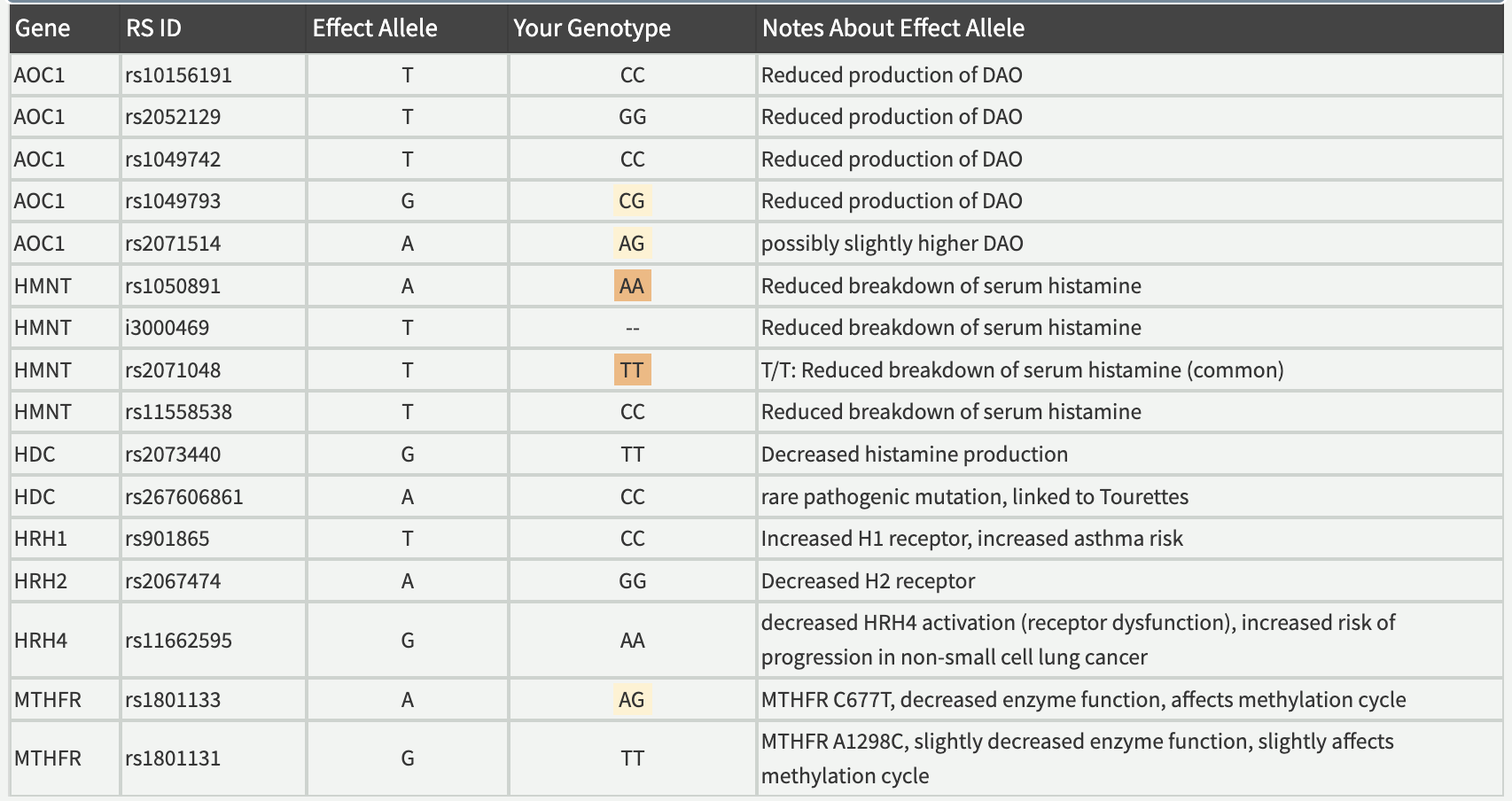
Here’s a sample of what you will see about your genes as a member:
Lifehacks: Diet and Supplements for MTHFR
Increase folate-rich foods:
The RDA for folate is 400 mcg/day. Increasing your intake of folate (vitamin B9) from foods will help mitigate some of the risks from the MTHFR variant.
Folate-rich foods include dark leafy greens, lentils, liver, asparagus, and broccoli.
If your diet doesn’t provide enough of the nutrients needed in the methylation cycle, you may want to consider supplements to increase your intake.
- Methylfolate: If you aren’t getting enough folate from foods, methylfolate is available as a supplement. Methylfolate is the active form of folate (vitamin B9).
- Vitamin B12 is also important in the methylation cycle, so you need to ensure you are getting enough B12 either through your diet (animal-based foods) or supplements. The ability to absorb B12 from the diet often decreases in aging, so supplemental forms may be a good option in older adults. (Also check your Vitamin B12 genes)
Side effects from methylfolate or methylB12:
Some people may find that methylfolate makes them irritable, irrationally angry, or anxious due to rapid changes in their neurotransmitter levels. People with the slow COMT genetic variant may want to be careful about high-dose supplements that affect the methylation cycle, such as methylfolate and methyl B12 (methylcobalamin). Instead, stick with dietary folate and use alternative forms of B12, such as adenosyl and hydroxocobalamin.
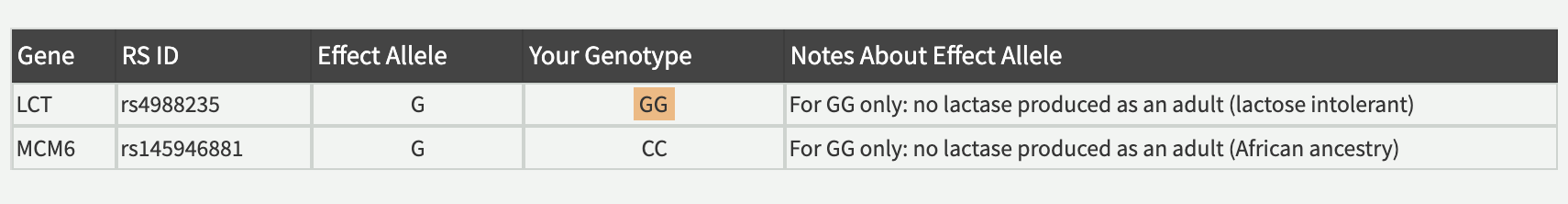
3. Dairy (LCT gene)
Lactose, a sugar in milk, is broken down by lactase, which is an enzyme produced in the small intestines.
While it is essential for babies and children to be able to break down lactose in breast milk, for many people, the production of the lactase enzyme stops before adulthood.
Whether or not you still produce lactase as an adult is based on your genes. A genetic variation near the LCT gene drives the persistence of lactase.
Thus, many adults are genetically predisposed not to be able to digest larger quantities of milk, also known as lactose intolerance. Others may be able to consume all the dairy that they wish to with no digestive problems.
The percentage of the population with genetic variations differs quite a bit among people with different ancestry.
- Producing lactase as an adult is the most common genotype for European Caucasian populations (90%+ can digest lactose).
- In Asian populations, the vast majority (~99%) do not produce lactase as an adult.
Historical and ancestry perspective:
A theory for differences in population percentages seems to be an adaptation by Caucasian populations in Europe who relied on dairy products as a source of protein. People born with the LCT variant could thrive – or more easily survive in tough times – on the higher protein contained in dairy products. This made it a survival advantage to digest dairy, but only in areas where sheep and cattle were used for milk.
For people with European Caucasian ancestry, the main variant (SNP) to look at is rs4988235. It is located in the MCM6 gene, which influences the LCT gene. Approximately 90% of Caucasians will have A/A or A/G and still produce lactase to break down milk as an adult. In people with Asian ancestry, less than one percent will carry the G allele.
The adaptation of the LCT gene to continue producing lactase into adulthood is one that came about through different variants in different population groups. In other words, a different mutation that allowed lactase persistence arose and became prevalent in people with African ancestry and then in Middle Eastern ancestry.
People with African ancestry may find that they carry a different variant in the MCM6 gene that also causes lactase persistence as an adult. (In the Genotype Report section below)
Bacteria in the gut can also break down lactose, so even people who don’t produce lactase as an adult can often handle digesting limited amounts of milk. This is going to be contingent on your gut microbiome and how often you consume milk products.
Lifehacks for Lactose Intolerance
Just because you are genetically not producing lactase as an adult doesn’t mean that you can’t digest any lactose. Instead, this means that you are relying on your gut microbiome to break down the lactose. Exceeding the amount that your gut microbiome can handle at one time is what causes ‘gastrointestinal distress’.
Quite a few studies have looked at the effect of probiotics on lactose intolerance. For example, a study found that a specific strain of Lactobacillus acidophilus significantly reduced the symptoms of lactose intolerance. [ref]
There are many species of Lactobacillus bacteria available as probiotics, and you can also get Lactobacillus in yogurt or other fermented dairy foods. Some strains will likely be more effective than others in reducing lactose intolerance symptoms for an individual. Thus, it may be worthwhile to try several different types of Lactobacillus sp. probiotics.
Include a little milk each day:
Regularly consuming some dairy (lactose) feeds your lactose-loving gut bacteria. A study found that consuming lactose for 10 days straight allowed for the colon microbiome to adapt to it. [ref] Thus, a moderate amount of cheese each day or milk in your coffee each morning will keep your Lactobacillus bacteria happily living in your gut microbiome, ready to take care of any lactose you consume.
Lactase enzyme supplements:
In most countries, you can buy the lactase enzyme in health food stores and take it along with foods containing dairy. Simply take the enzymes before your dairy-containing meal and the lactase enzyme will be available in your gut to break down the lactose in the dairy.
Lactose-free dairy products are also readily available. Often these are made by adding lactase enzymes to the product.
4. Histamine in Foods (check the HNMT or AOC1 gene)
Histamine intolerance symptoms impact many different systems in the body, including[ref]:
- Head: headaches & migraines
- Mood: anxiety, irritability, brain fog
- Stomach: acid reflux, nausea, stomach pain
- Intestines: bloating, diarrhea, constipation
- Heart: heart arrhythmia, dizziness
- Sinuses: drainage, congestion
- Skin: hives, weal, itching, flushing,
- Sleep: insomnia, early waking
People with histamine intolerance usually have several of the symptoms above, but they likely won’t have all of the symptoms.[ref]
The two leading causes of histamine intolerance are:
- not enough of the enzymes needed to break down histamine (DAO and HMNT)
– and/or- - too much histamine being produced (gut microbes producing histamine, leaky gut, mast cells degranulating too easily, HDC variants, chronic exposure to allergens).
There are two ways your body breaks down and clears histamine: the DAO enzyme or the HMNT enzyme.[ref]
- Diamine oxidase (DAO) enzyme: Histamine from foods or bacteria in your gut is broken down or metabolized using the DAO (diamine oxidase) enzyme. The DAO enzyme is produced in the villi lining the small intestines and is released to metabolize histamine.[ref]
- Histamine methyltransferase (HMNT) enzyme: The HMNT enzyme works throughout the body, including in the brain, to deactivate and break down histamine created by your cells.[ref]
DAO (diamine oxidase) is the enzyme produced by the intestines, breaking down histamine from foods. The AOC1 gene codes for the production of the DAO enzyme. Genetic variants in AOC1 can increase or decrease the production of the enzyme.
Histamine n-methyltransferase (HMNT) is the enzyme that regulates histamine in the body by converting it from histamine into N-methylhistamine, which can then be eliminated from the body. HNMT is responsible for eliminating 80% of histamine in the body.[ref]
The methylation cycle plays a role in breaking down monoamine neurotransmitters, including histamine. It is also important in creating the methyl groups needed for the HMNT enzyme to work. So looking at your methylation cycle genes can also help with balancing out histamine intolerance.
The MTHFR gene codes for an enzyme that is a key player in the folate cycle. It is one source of methyl groups for the methylation cycle. Decreased enzyme activity of MTHFR – combined with a diet lacking in folate or choline – may cause a reduced breakdown of histamine.
Lifehacks for histamine intolerance:
Low-histamine diet:
In general, foods that are fermented or aged are higher in histamine. High histamine foods include processed meats, cheeses (except farmer cheese), fish and seafood that isn’t completely fresh, spinach, chocolate, tomatoes, strawberries, wine, sake, and more.
Research on supplements for Histamine Intolerance:
Vitamin B6 is a cofactor in the reactions that degrade histamine.[ref] Pyridoxal-5′-phosphate is the active form of vitamin B6. Foods high in vitamin B6 include salmon, tuna, eggs, milk, beef, and carrots. (article) Not sure if you get enough vitamin B6? Cronometer.com is a free online app where you can record the foods you eat each day to determine the nutrient content – and it includes the vitamin B6 content of foods.
Quercetin has also been shown in studies to inhibit mast cells from degranulating. Mast cells are one way that the body releases histamine.[ref]
Fisetin, another natural flavonol, has been shown in cell studies to inhibit mast cells from degranulating.[ref][ref][ref](Read more about fisetin)
Luteolin has been shown in studies to inhibit histamine release from mast cells.[ref]
There are DAO supplements available that may help some people who don’t produce enough of the enzyme. A recent study found that histamine intolerance symptoms improved significantly when taking DAO capsules before meals.[ref]
Looking for an alternative to expensive DAO supplements? Pea shoots – those first few inches of the pea plant that come up in the spring – are naturally high in the DAO enzyme.[ref]
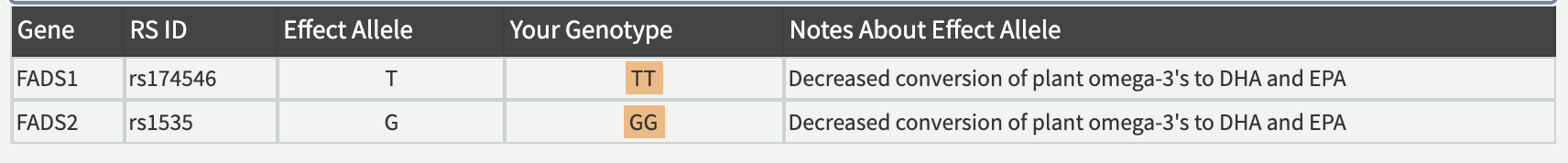
5. Fish oil vs. Flaxseed (check the FADS1 and FADS2 genes)
Fatty acids, including both saturated and polyunsaturated fats, make up the membrane surrounding each cell in the body. The body also uses omega-6 and omega-3 fatty acids to make eicosanoids (pro- and anti-inflammatory molecules), pro-resolving lipid mediators, endocannabinoids, and cellular signaling molecules.
While both omega 6 and omega 3 fats are essential, there has been a recent shift in how much omega 6 fats are in our diets.
The metabolism of both the omega-6 and omega-3 fatty acids involves the same FADS1 and FADS2 enzymes.
This is where the ratio of omega-3 to omega-6 fats in your diet comes into play. With only a limited amount of these desaturase enzymes available, a high ratio of omega-6 to omega-3 means more of the omega-6 will be metabolized into arachidonic acid, and less EPA and DHA will be produced.
The FADS1 (encodes delta-5 desaturase) and FADS2 (encodes delta-6 desaturase) genes have several different variants that slow down the production of the enzymes. There are multiple FADS1 variants that are inherited together such that if you inherit one, you should inherit all the variants.
Studies on the linked FADS1 variants that decrease enzyme activity – rs174546 (T ), rs174547 (C), 174537 (T), and rs174548 (G) show:
- People carrying the low activity variant had decreased LDL levels when they had low consumption of omega-3 fatty acids.[ref]
- Lower arachidonic acid and EPA levels[ref]
- Lower risk of type 2 diabetes[ref]
- Arachidonic acid and phosphatidylcholine are reduced[ref]
- lower HDL, lower glucose, but higher triglycerides[ref]
Lifehacks for FADS1 & 2:
Our modern diets tend to be high in omega-6 oils, which you may want to decrease if it is out of balance with the amount of omega-3 fats you consume.
Foods high in these oils include most mayonnaises, salad dressings, margarine, walnuts, sunflower seeds, and peanut butter. Pretty much anything that is fried is high in omega-6 oils.[ref]
Foods and oils that are high in omega-3, which you may want to increase, include:
- fish oil (DHA, EPA)
- fatty fish
- seal oil
- flax seed (alpha-linolenic acid) (must be converted with FADS enzyme)
- chia seeds (must be converted with FADS enzyme)
- caviar
With a Genetic Lifehacks membership, you can see your genes in all of these nutrient-related articles — plus about 400 more interesting topics! Dive in and learn about how your genes impact your response to toxins, your susceptibility to metabolic problems, your risk for heart disease, and so much more.