Key takeaways:
~ Chronic inflammation is the driver of many common diseases, such as heart attacks, diabetes, obesity, and autoimmune diseases. The C-reactive protein (CRP) test is one way to know if you have chronic inflammation problems.
~ Some people have variants in the CRP gene that naturally elevate their CRP levels a little — others carry genetic variants that decrease their CRP levels.
~ Up to half of the variation seen in CRP levels is due to genetics.[ref]
What is C-reactive Protein (CRP)?
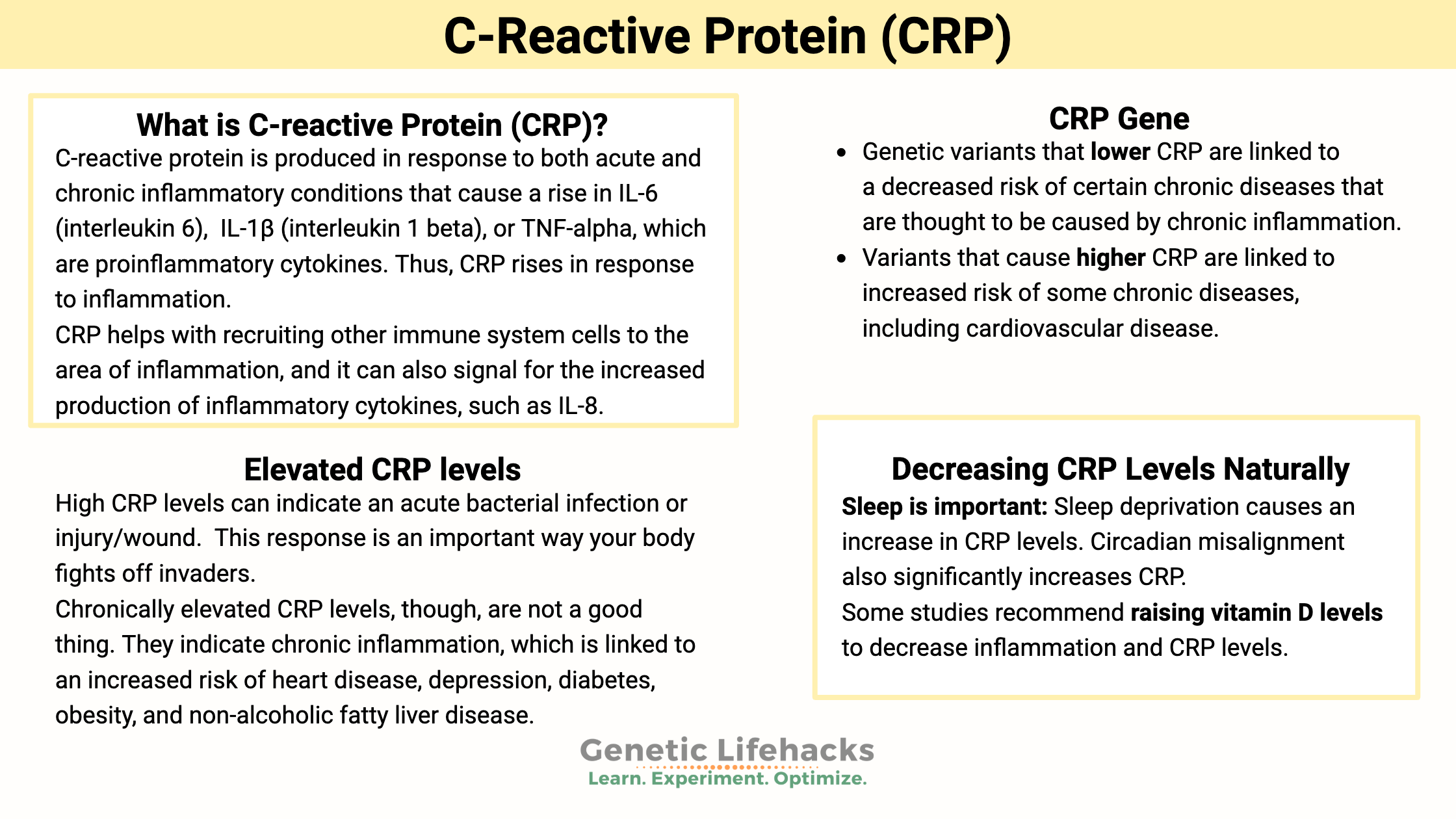
C-reactive protein is produced in response to both acute and chronic inflammatory conditions that cause a rise in IL-6 (interleukin 6), IL-1β (interleukin 1 beta), or TNF-alpha, which are proinflammatory cytokines. The liver (primarily) detects the increase in the inflammatory cytokines and synthesizes CRP. Thus, CRP rises in response to inflammation.[ref]
CRP levels were initially identified just as a marker of inflammation, but more recent research shows that CRP plays an important role in inflammatory processes and in the response to infections.
The “C” in C-reactive protein comes from the initial discovery that it was produced in response to the C polysaccharide found on the cell wall of pneumococcus bacteria. CRP binds to phosphocholine on bacteria or dead cells as a marker that they need to be cleared out.
When inflammation arises somewhere in the body, the liver detects the elevated IL-6 and produces CRP as part of the acute-phase response. CRP helps with recruiting other immune system cells to the area of inflammation, and it can also signal for the increased production of inflammatory cytokines, such as IL-8. [ref]
Elevated CRP levels:
CRP is easily measured in the blood and is a commonly used lab test to see if there is acute or chronic inflammation in the body. In addition, it is a steady marker of inflammation – it doesn’t fluctuate with food intake or with the time of day.[ref]
High CRP levels can indicate an acute bacterial infection or injury/wound. CRP levels can rise 1,000 – 2,000-fold in just hours as an acute response to a pathogen. This response is an important way your body fights off invaders.[ref]
Chronically elevated CRP levels, though, are not a good thing. They indicate chronic inflammation linked to an increased risk of heart disease, depression, diabetes, obesity, and non-alcoholic fatty liver disease.[ref][ref][ref][ref][ref]
CRP levels on tests:
CRP is tested to see if there is an ongoing inflammatory condition and it is used by some doctors to assess the risk of cardiovascular disease.
- Normal C-reactive protein levels are below 3.0 mg/L.
- Over 3.0 mg/L is considered ‘high’ and is used by doctors to determine heart health risk.
- CPR levels can reach levels of over 100 mg/L in situations of active, acute inflammation.
hs-CRP (high sensitivity CRP) is a more precise test used to determine chronic inflammation and heart disease risk. Elevated levels (usually >3.0 mg/L, but some studies use 2.0 mg/L) are associated with an increased risk of atherosclerosis and coronary artery disease due to increasing inflammation in the blood vessel and promoting clotting.[ref]
Is high CRP genetic?
Genetics plays a role in your propensity towards higher or lower baseline levels of CRP. For example, if your CRP level is on the high end of normal, it may be that genetically you tend to produce more CRP.
To some extent, the link between the genetic variants and disease helps to answer whether CRP is just a ‘marker of inflammation’ or plays a role in causing the disease.
- Genetic variants that lower CRP are linked to a decreased risk of certain chronic diseases that are thought to be caused by chronic inflammation.
- Variants that cause higher CRP are linked to increased risk of some chronic diseases, including cardiovascular disease.[ref]
Studies showing that CRP may be ‘causal’:
- In heart disease, CRP may be actively causing atherosclerosis (hardening of the arteries)[ref], thus the increased risk of heart disease.
- It is also theorized that higher CRP levels may affect fat cells and increase weight.[ref]
- For type 2 diabetes, researchers found that variants linked to an increase in CRP are also linked to an increased risk of diabetes.[ref]
But other studies show that genetically higher CRP levels may not always cause diseases associated with chronic inflammation.
- A study looking at the link between higher CRP levels in people with depression found that the genetic variants linked to higher CRP were likely not causal in depression. Instead, the researchers concluded that “CRP may be a compensatory response to external insults that predispose to depression and that an increase in the concentration of CRP might be adaptive.”[ref]
CRP Genotype Report
Access this content:
An active subscription is required to access this content.
Lifehacks:
In general, lower CRP levels should indicate lower levels of chronic inflammation. You can get your doctor to order a CRP blood test for you, or you can order it yourself through an online lab company.
Decreasing CRP levels naturally:
The following suggestions are based on studies showing decreases in CRP levels.
Cut out trans fats:
A study of 730 nurses found that those who ate higher levels of trans fats had 73% higher CRP levels.[ref] This is an easy change to make, and trans-fats have a variety of negative health effects, so you should cut them out even if your CRP is not a problem.
Exercise (the right amount):
Access this content:
An active subscription is required to access this content.
Summing this all up:
Higher CRP levels increase the risk of heart disease and other chronic diseases. Your genetic variants may be playing a role in your CRP levels. The best dietary advice includes olive oil, garlic, and a Mediterranean-style diet with fresh veggies — along with red wine. Sleeping is essential, and so is moderate exercise in the sunshine. Sounds like a trip to the Greek Isles is just what the doctor should order!
Related Articles and Topics:
Lipoprotein (a)
High Lp(a) levels are a big risk factor for sudden heart attacks. Your Lp(a) levels are mainly controlled by your genetic variants. Check to see if you carry genetic variants that increase or decrease Lp(a).
TNF-Alpha: Inflammation and Your Genes
Do you feel like you are always dealing with inflammation? Joint pain, food sensitivity, etc.? Perhaps you are genetically geared towards a higher inflammatory response. Tumor necrosis factor (TNF) is an inflammatory cytokine that acts as a signaling molecule in our immune system.
Inflammation: Causes and Natural Solutions
Take a deep dive into the causes of chronic inflammation and learn how to target specific inflammatory pathways to reverse or prevent chronic disease.
Specialized Pro-resolving Mediators: Getting Rid of Chronic Inflammation
Chronic inflammation is at the root of all diseases. New research discusses how pro-resolving mediators are the key to the resolution of inflammation.
References:
Almeida, Osvaldo P., et al. “Polymorphisms of the CRP Gene Inhibit Inflammatory Response and Increase Susceptibility to Depression: The Health in Men Study.” International Journal of Epidemiology, vol. 38, no. 4, Aug. 2009, pp. 1049–59. PubMed, https://doi.org/10.1093/ije/dyp199.
Badawi, Alaa, et al. “Type 2 Diabetes Mellitus and Inflammation: Prospects for Biomarkers of Risk and Nutritional Intervention.” Diabetes, Metabolic Syndrome and Obesity : Targets and Therapy, vol. 3, May 2010, pp. 173–86. PubMed Central, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3047967/.
Bahmani, Fereshteh, et al. “The Effects of Folate Supplementation on Inflammatory Factors and Biomarkers of Oxidative Stress in Overweight and Obese Women with Polycystic Ovary Syndrome: A Randomized, Double-Blind, Placebo-Controlled Clinical Trial.” Clinical Endocrinology, vol. 81, no. 4, Oct. 2014, pp. 582–87. PubMed, https://doi.org/10.1111/cen.12451.
Berk, Michael, et al. “Aspirin: A Review of Its Neurobiological Properties and Therapeutic Potential for Mental Illness.” BMC Medicine, vol. 11, Mar. 2013, p. 74. PubMed Central, https://doi.org/10.1186/1741-7015-11-74.
Chen, Xiao-Lin, et al. “Genotype CC of Rs1800947 in the C-Reactive Protein Gene May Increase Susceptibility to Colorectal Cancer: A Meta-Analysis.” Asian Pacific Journal of Cancer Prevention: APJCP, vol. 15, no. 6, 2014, pp. 2663–67. PubMed, https://doi.org/10.7314/apjcp.2014.15.6.2663.
Crawford, Dana C., et al. “Genetic Variation Is Associated with C-Reactive Protein Levels in the Third National Health and Nutrition Examination Survey.” Circulation, vol. 114, no. 23, Dec. 2006, pp. 2458–65. PubMed, https://doi.org/10.1161/CIRCULATIONAHA.106.615740.
Della Corte, Karen W., et al. “Effect of Dietary Sugar Intake on Biomarkers of Subclinical Inflammation: A Systematic Review and Meta-Analysis of Intervention Studies.” Nutrients, vol. 10, no. 5, May 2018, p. 606. PubMed Central, https://doi.org/10.3390/nu10050606.
Estruch, Ramon, et al. “Different Effects of Red Wine and Gin Consumption on Inflammatory Biomarkers of Atherosclerosis: A Prospective Randomized Crossover Trial. Effects of Wine on Inflammatory Markers.” Atherosclerosis, vol. 175, no. 1, July 2004, pp. 117–23. PubMed, https://doi.org/10.1016/j.atherosclerosis.2004.03.006.
Gao, Xiu-Ren, et al. “Efficacy of Different Doses of Aspirin in Decreasing Blood Levels of Inflammatory Markers in Patients with Cardiovascular Metabolic Syndrome.” The Journal of Pharmacy and Pharmacology, vol. 61, no. 11, Nov. 2009, pp. 1505–10. PubMed, https://doi.org/10.1211/jpp/61.11.0010.
Gawron-Skarbek, Anna, et al. “Dietary Vitamin C, E and β-Carotene Intake Does Not Significantly Affect Plasma or Salivary Antioxidant Indices and Salivary C-Reactive Protein in Older Subjects.” Nutrients, vol. 9, no. 7, July 2017, p. 729. PubMed Central, https://doi.org/10.3390/nu9070729.
Hall, Martica H., et al. “Sleep Duration during the School Week Is Associated with C-Reactive Protein Risk Groups in Healthy Adolescents.” Sleep Medicine, vol. 16, no. 1, Jan. 2015, pp. 73–78. PubMed, https://doi.org/10.1016/j.sleep.2014.10.005.
Hernández-Díaz, Yazmín, et al. “The Role of Gene Variants of the Inflammatory Markers CRP and TNF-α in Cardiovascular Heart Disease: Systematic Review and Meta-Analysis.” International Journal of Clinical and Experimental Medicine, vol. 8, no. 8, 2015, pp. 11958–84.
Huang, Yu-Chuen, et al. “C-Reactive Protein Gene Variants and Their Serum Levels in Early Adult-Onset Type 2 Diabetes Mellitus.” In Vivo (Athens, Greece), vol. 33, no. 5, Oct. 2019, pp. 1685–90. PubMed, https://doi.org/10.21873/invivo.11656.
Irwin, Michael R., et al. “Sleep Disturbance, Sleep Duration, and Inflammation: A Systematic Review and Meta-Analysis of Cohort Studies and Experimental Sleep Deprivation.” Biological Psychiatry, vol. 80, no. 1, July 2016, pp. 40–52. PubMed, https://doi.org/10.1016/j.biopsych.2015.05.014.
Jonasson, Lena, et al. “Advice to Follow a Low-Carbohydrate Diet Has a Favourable Impact on Low-Grade Inflammation in Type 2 Diabetes Compared with Advice to Follow a Low-Fat Diet.” Annals of Medicine, vol. 46, no. 3, May 2014, pp. 182–87. PubMed Central, https://doi.org/10.3109/07853890.2014.894286.
Kronish, Ian M., et al. “Aspirin Adherence, Aspirin Dosage, and C-Reactive Protein in the First Three Months after an Acute Coronary Syndrome.” The American Journal of Cardiology, vol. 106, no. 8, Oct. 2010, pp. 1090–94. PubMed Central, https://doi.org/10.1016/j.amjcard.2010.06.018.
Lim, Soo, et al. “The Relationship between Body Fat and C-Reactive Protein in Middle-Aged Korean Population.” Atherosclerosis, vol. 184, no. 1, Jan. 2006, pp. 171–77. PubMed, https://doi.org/10.1016/j.atherosclerosis.2005.04.003.
MacGregor, Alex J., et al. “Genetic Effects on Baseline Values of C-Reactive Protein and Serum Amyloid a Protein: A Comparison of Monozygotic and Dizygotic Twins.” Clinical Chemistry, vol. 50, no. 1, Jan. 2004, pp. 130–34. PubMed, https://doi.org/10.1373/clinchem.2003.028258.
Mahajan, Anubha, et al. “Common Variants in CRP and LEPR Influence High Sensitivity C-Reactive Protein Levels in North Indians.” PLoS ONE, vol. 6, no. 9, Sept. 2011, p. e24645. PubMed Central, https://doi.org/10.1371/journal.pone.0024645.
Mirhosseini, Naghmeh, et al. “Vitamin D Supplementation, Serum 25(OH)D Concentrations and Cardiovascular Disease Risk Factors: A Systematic Review and Meta-Analysis.” Frontiers in Cardiovascular Medicine, vol. 5, July 2018, p. 87. PubMed Central, https://doi.org/10.3389/fcvm.2018.00087.
Myburgh, Pieter H., et al. “CRP Genotypes Predict Increased Risk to Co-Present with Low Vitamin D and Elevated CRP in a Group of Healthy Black South African Women.” International Journal of Environmental Research and Public Health, vol. 15, no. 1, Jan. 2018, p. 111. PubMed Central, https://doi.org/10.3390/ijerph15010111.
Nimptsch, Katharina, et al. “Association of CRP Genetic Variants with Blood Concentrations of C-Reactive Protein and Colorectal Cancer Risk.” International Journal of Cancer, vol. 136, no. 5, Mar. 2015, pp. 1181–92. PubMed Central, https://doi.org/10.1002/ijc.29086.
Okada, Yukinori, et al. “Genome-Wide Association Study for C-Reactive Protein Levels Identified Pleiotropic Associations in the IL6 Locus.” Human Molecular Genetics, vol. 20, no. 6, Mar. 2011, pp. 1224–31. PubMed, https://doi.org/10.1093/hmg/ddq551.
Perry, Tjörvi E., et al. “C-Reactive Protein Gene Variants Are Associated with Postoperative C-Reactive Protein Levels after Coronary Artery Bypass Surgery.” BMC Medical Genetics, vol. 10, May 2009, p. 38. PubMed Central, https://doi.org/10.1186/1471-2350-10-38.
Potter, Gregory D. M., et al. “Longer Sleep Is Associated with Lower BMI and Favorable Metabolic Profiles in UK Adults: Findings from the National Diet and Nutrition Survey.” PLoS ONE, vol. 12, no. 7, July 2017, p. e0182195. PubMed Central, https://doi.org/10.1371/journal.pone.0182195.
Rajaie, Somayeh, et al. “Comparative Effects of Carbohydrate versus Fat Restriction on Serum Levels of Adipocytokines, Markers of Inflammation, and Endothelial Function among Women with the Metabolic Syndrome: A Randomized Cross-over Clinical Trial.” Annals of Nutrition & Metabolism, vol. 63, no. 1–2, 2013, pp. 159–67. PubMed, https://doi.org/10.1159/000354868.
Ridker, Paul M., et al. “Loci Related to Metabolic-Syndrome Pathways Including LEPR,HNF1A, IL6R, and GCKR Associate with Plasma C-Reactive Protein: The Women’s Genome Health Study.” American Journal of Human Genetics, vol. 82, no. 5, May 2008, pp. 1185–92. PubMed Central, https://doi.org/10.1016/j.ajhg.2008.03.015.
Schwingshackl, L., and G. Hoffmann. “Mediterranean Dietary Pattern, Inflammation and Endothelial Function: A Systematic Review and Meta-Analysis of Intervention Trials.” Nutrition, Metabolism, and Cardiovascular Diseases: NMCD, vol. 24, no. 9, Sept. 2014, pp. 929–39. PubMed, https://doi.org/10.1016/j.numecd.2014.03.003.
Schwingshackl, Lukas, et al. “Effects of Olive Oil on Markers of Inflammation and Endothelial Function-A Systematic Review and Meta-Analysis.” Nutrients, vol. 7, no. 9, Sept. 2015, pp. 7651–75. PubMed, https://doi.org/10.3390/nu7095356.
Shen, Jian, and Jose M. Ordovas. “Impact of Genetics and Environmental Factors on CRP Levels and Response to Therapeutic Agents.” Clinical Chemistry, vol. 55, no. 2, Feb. 2009, pp. 256–64. PubMed Central, https://doi.org/10.1373/clinchem.2008.117754.
Song, Xiaoling, et al. “A Low-Fat High-Carbohydrate Diet Reduces Plasma Total Adiponectin Concentrations Compared to a Moderate-Fat Diet with No Impact on Biomarkers of Systemic Inflammation in a Randomized Controlled Feeding Study.” European Journal of Nutrition, vol. 55, no. 1, Feb. 2016, pp. 237–46. PubMed, https://doi.org/10.1007/s00394-015-0841-1.
Stancel, Nicole, et al. “Interplay between CRP, Atherogenic LDL, and LOX-1 and Its Potential Role in the Pathogenesis of Atherosclerosis.” Clinical Chemistry, vol. 62, no. 2, Feb. 2016, pp. 320–27. PubMed, https://doi.org/10.1373/clinchem.2015.243923.
Sudhakar, Manu, et al. “C-Reactive Protein (CRP) and Leptin Receptor in Obesity: Binding of Monomeric CRP to Leptin Receptor.” Frontiers in Immunology, vol. 9, May 2018, p. 1167. PubMed Central, https://doi.org/10.3389/fimmu.2018.01167.
Sutliffe, Jay T., et al. “C-Reactive Protein Response to a Vegan Lifestyle Intervention.” Complementary Therapies in Medicine, vol. 23, no. 1, Feb. 2015, pp. 32–37. PubMed, https://doi.org/10.1016/j.ctim.2014.11.001.
Swardfager, Walter, et al. “Exercise Intervention and Inflammatory Markers in Coronary Artery Disease: A Meta-Analysis.” American Heart Journal, vol. 163, no. 4, Apr. 2012, pp. 666-676.e1-3. PubMed, https://doi.org/10.1016/j.ahj.2011.12.017.
Talikoti, Prashanth, et al. “Hyperhomocysteinemia, Insulin Resistance and High HS- CRP Levels in Prehypertension.” Journal of Clinical and Diagnostic Research: JCDR, vol. 8, no. 8, Aug. 2014, pp. CC07-09. PubMed, https://doi.org/10.7860/JCDR/2014/8945.4669.
Torres, A., et al. “Red Wine Intake but Not Other Alcoholic Beverages Increases Total Antioxidant Capacity and Improves Pro-Inflammatory Profile after an Oral Fat Diet in Healthy Volunteers.” Revista Clinica Espanola, vol. 215, no. 9, Dec. 2015, pp. 486–94. PubMed, https://doi.org/10.1016/j.rce.2015.07.002.
Wright, Kenneth P., et al. “Influence of Sleep Deprivation and Circadian Misalignment on Cortisol, Inflammatory Markers, and Cytokine Balance.” Brain, Behavior, and Immunity, vol. 47, July 2015, pp. 24–34. PubMed, https://doi.org/10.1016/j.bbi.2015.01.004.