Key takeaways:
~ Milk allergy is a common IgE food allergy and can involve casein or β-lactoglobulin sensitivity.
~ Nanoparticles interact with milk proteins to increase allergenicity.
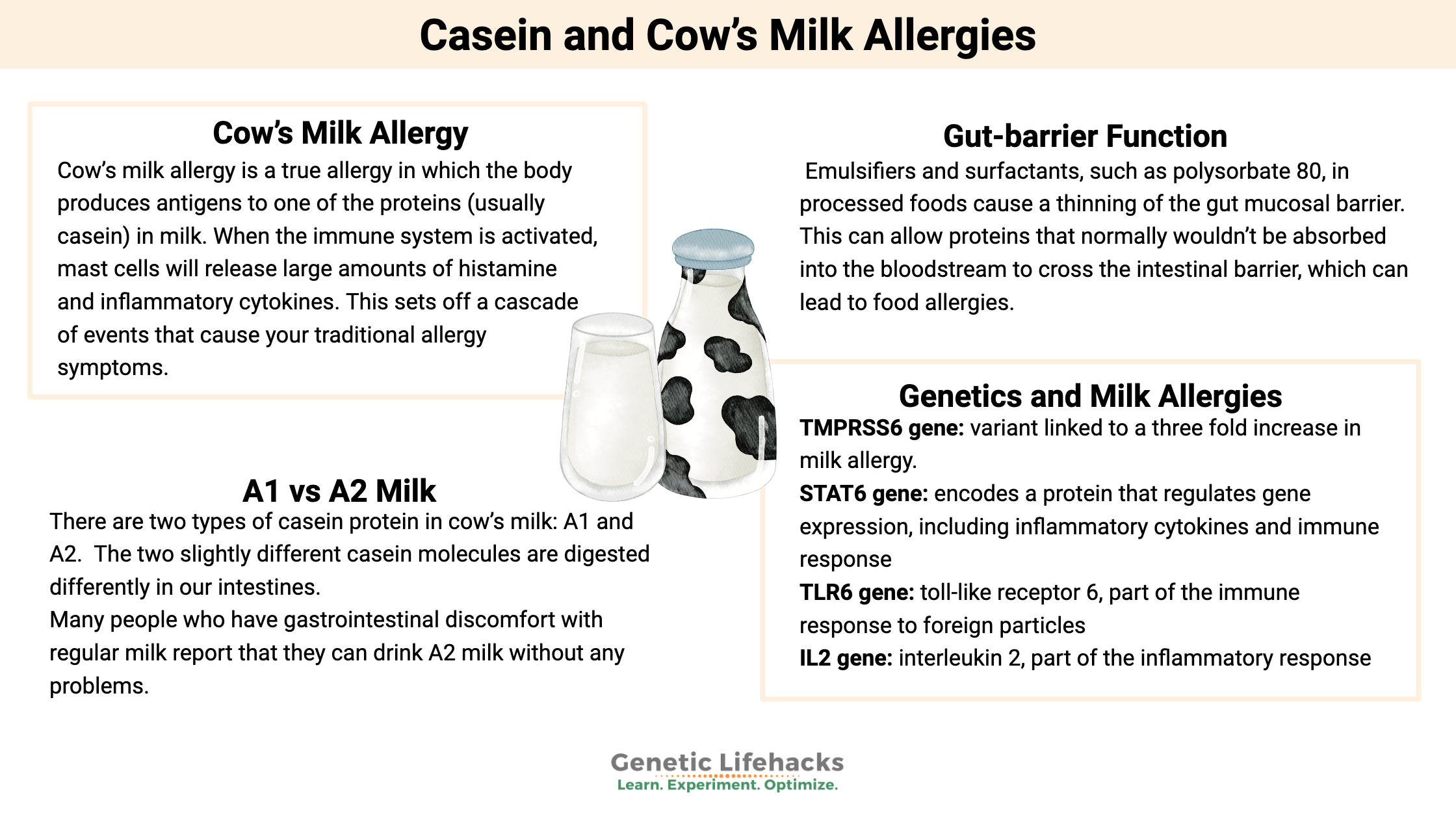
~ Genetic variants in immune system genes increase susceptibility to milk allergy.
What is a milk allergy? And how do your genes increase the risk?
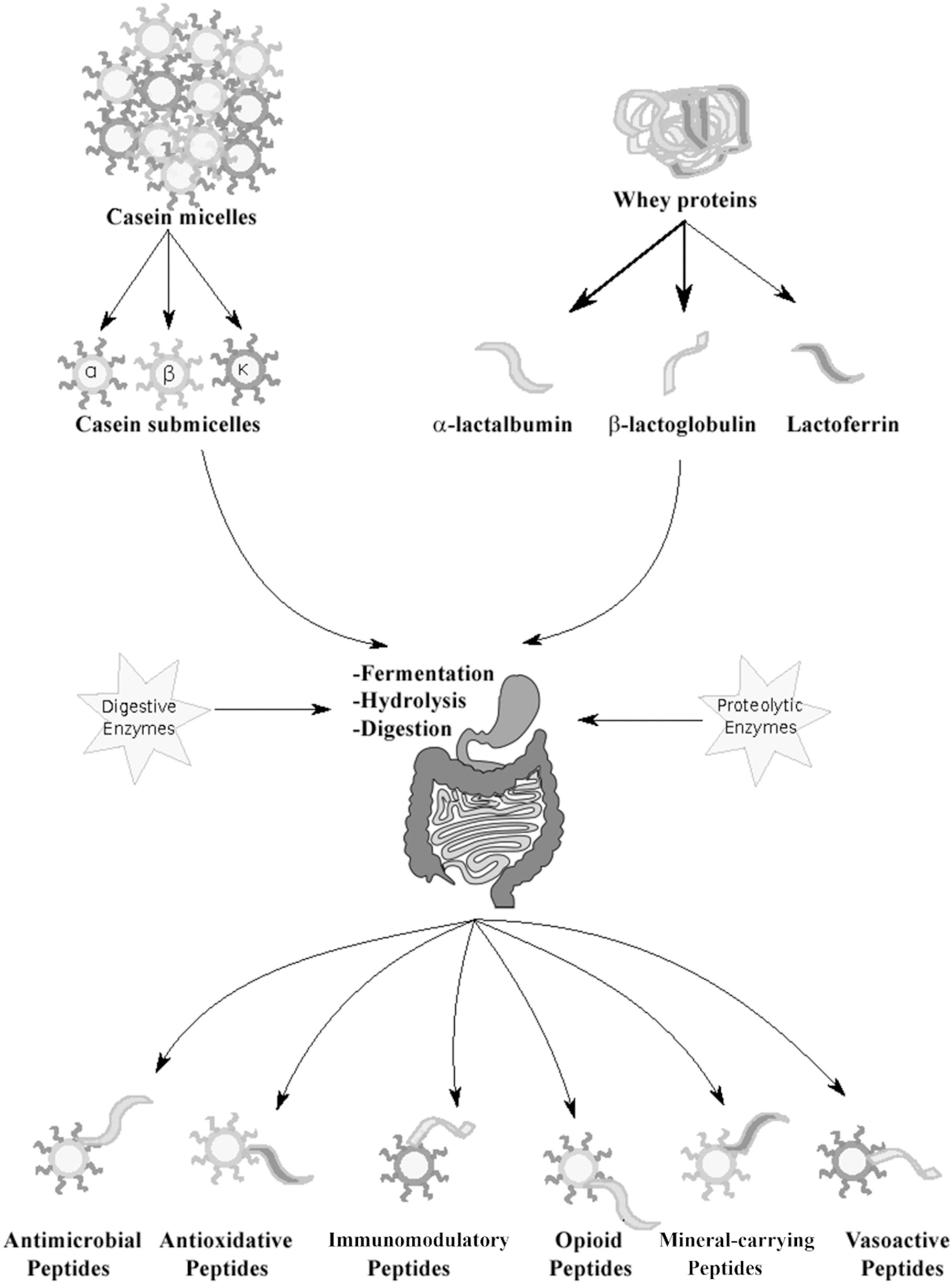
Cow’s Milk Allergy (CMA) is a term used to describe a reaction to cow’s milk proteins, specifically casein or β-lactoglobulin. This is different from lactose intolerance, which is an inability to break down the sugar lactose in milk. Both cow’s milk allergy and lactose intolerance are used to describe a wide range of gastrointestinal symptoms associated with the consumption of milk and dairy products.
With the availability of lactose-free milk options, most people can determine if the problem is lactose or if it is one of the proteins in the milk. While most children have the ability to break down lactose by producing the lactase enzyme, the ability to produce lactase as an adult varies greatly by ancestry.
Related article: Lactase persistence
Cow’s milk allergy is a true allergy in which the body produces antigens to one of the proteins (usually casein) in milk. When the immune system is activated, mast cells will release large amounts of histamine and inflammatory cytokines. This sets off a cascade of events that cause your traditional allergy symptoms.[ref]
Cow’s milk allergy is most common in infants and children, with 50-90% outgrowing the allergy as they grow older.[ref]
Symptoms of milk allergy include:[ref]
- Hives or wheezing
- Swelling lips and tongue; itchy, tingly feeling around the lips; anaphylaxis
- Diarrhea, abdominal cramps, upset stomach
- Runny nose, watery eyes
What has caused the increased risk of milk allergies?
Allergies seem to be on the rise these days, and there are many theories as to why. Humans have been consuming cow’s milk for over 5,000 years. Yet milk allergies are now common in infants and children. Milk processing has changed over the last hundred years, and heat treatments alter the structure of the milk proteins a bit.[ref] This altered milk protein structure interacts with other food additives in our modern diet.
For milk allergy, research shows the following may interact with milk proteins to increase allergy risk:
- Nanoparticles, such as silicon dioxide or titanium dioxide
- Microplastics and nanoplastics
- Emulsifiers that cause changes in the intestinal mucosal barrier
Nanoparticles added to foods:
Inorganic nanoparticles are added to a lot of processed foods, spices, and infant formulas — as well as many “natural” supplements. Keep in mind that for a breastfed infant, these nanoparticles can be passed along to the baby.[ref][ref]
- In mice, food-grade titanium dioxide, which is a common food additive, increases the propensity for food allergies including milk allergy.[ref]
- Silicon dioxide also increases the propensity for milk allergy. Silicon dioxide nanoparticles “enhance antigenicity and allergenicity of milk proteins.”[ref]
Silicon dioxide is added as an anti-caking agent to many powdered foods, such as spices or drink mixes. It is also commonly found in dietary supplements, dehydrated powders, chewing gum, and processed foods. Studies show that in addition to altering milk proteins, silica also causes low-grade inflammation in the gut.[ref]
Nanoplastics:
Research shows that microplastics and nanoplastics may increase susceptibility to food allergies in several ways. For milk allergies, studies show that microscopic pieces of polystyrene can interact with the protein structure in milk to increase its allergenicity.[ref][ref]
Gut-barrier function and milk allergies:
While not specific to milk allergy, there’s quite a bit of research showing that emulsifiers and surfactants, such as polysorbate 80, in processed foods cause a thinning of the gut mucosal barrier. This can allow proteins that normally wouldn’t be absorbed into the bloodstream to cross the intestinal barrier (leaky gut), which can lead to food allergies.[ref][ref]
Related article: Leaky gut genes: Emulsifiers in processed foods
In addition to interacting with milk proteins, nanoparticles like silicon dioxide and silver nanoparticles loosen the tight junctions in the intestines, further exacerbating their interaction with milk allergy.[ref][ref]
A1 vs A2 Milk: Two types of casein
While the changes in the processing of milk and an increase in food additives are part of the increase in milk allergy, another somewhat recent change in milk is in the amino acid composition of casein.
Casein, or more specifically β-casein, makes up about 30% of the total protein in milk.
There are two types of casein protein in cow’s milk: A1 and A2. Just as we have SNPs that make us unique, cows have SNPs that cause them to produce two variants of casein. The two slightly different casein molecules are digested differently in our intestines.
Certain breeds of cows, including Holstein, Friesian, and British Shorthorn, typically produce A1 milk (or A1/A2 milk), while Guernsey, Jersey, Simmental (Swiss), Charolais, Limousin, and indigenous Asian breeds, produce A2 β-casein.[ref]
A1 casein is more likely to undergo enzymatic cleavage in the intestines. This cleavage produces a peptide β-casomorphin-7 (BCM-7), which can bind to the μ-opioid receptor.[ref] The μ-opioid (mu-opioid) receptor is found in the brain, spinal cord, and intestines. This is the receptor to which opioid drugs bind to relieve pain.
Many people who have gastrointestinal discomfort with regular milk report that they can drink A2 milk without any problems. The difference seems to be the effect of the β-casomorphin-7 (BCM-7) peptide produced when the A1 casein is cleaved.
Some studies also suggest that the BCM-7 peptide may play a role in the neurocognitive development of children who drink A1 milk. Autistic children on a casein-free diet have reduced intestinal inflammation. However, there is no clear evidence that A1 milk and the BCM-7 peptide play a role in neurodevelopmental disorders.[ref]
The A1 casein protein has also been associated with diabetes and cardiovascular disease in epidemiologic and association studies.[ref]
Delayed-type hypersensitivity:
Some individuals have a non-IgE-mediated response to milk proteins – a hypersensitivity instead of a ‘true’ allergy with symptoms appearing hours after consuming milk. These types of reactions are much more difficult to diagnose since there isn’t a quick test to see the reaction. For example, eczema can be a symptom of non-IgE-mediated hypersensitivity to milk in infants, but not all eczema is caused by milk sensitivity.[ref] In infants, the non-IgE response to milk often takes the form of diarrhea and sometimes vomiting. This often resolves on its own within a year.[ref]
Misdiagnosis is common:
It can be really hard to know what is causing delayed hypersensitivity reactions, and milk or gluten are often removed from the diet without a solid diagnosis. A study in children who had been on a strict dairy-free or gluten-free diet showed that a double-blind placebo-controlled food challenge given at three different times could show who had delayed hypersensitivity. The study found that 75% of the children and teens in the study didn’t present with symptoms when reintroduced to the food in the double-blind challenge.[ref]
Genotype report: Milk or Casein Allergy
Access this content:
An active subscription is required to access this content.
Lifehacks:
Allergy testing:
If you suspect a milk allergy, the only way to know for sure is to get tested by an allergist. They can determine if you have a true IgE allergy or not and may be able to help determine hypersensitivity reactions as well. Note that this is not the same as food sensitivity testing, which measures IgG antibodies in the blood after exposure to a food. There’s a lot of controversy around whether IgG food sensitivity testing is valid, but wherever you land on that topic, it isn’t the same as allergy testing.
Avoiding casein:
Milk allergies are hard because casein is found in a lot of products. In addition to the obvious, like milk, cheese, and ice cream, look carefully at ingredient lists for casein, milk protein hydrolysate, whey protein, and cream solids.[ref] Godairyfree.org has an extensive list as well.
Slow low-dose oral immunotherapy:
A clinical trial of low-dose oral immunotherapy in children with severe cow’s milk allergy showed that about one-third of the children were desensitized after three years. [ref]
Papain:
Papain is an enzyme found in papaya that can reduce the allergenicity of casein.[ref][ref] I’m not sure how this could be used for drinking milk, since papain will cause milk to curdle or coagulate. Papain can be used to make cottage cheese….. However, this could be useful in milk that is used for cooking.
Yogurt:
A study in children with IgE-mediated milk allergies showed that about half of them were able to tolerate yogurt. Those that could tolerate yogurt had lower IgE levels toward cow’s milk.[ref] To be clear: I’m not suggesting that you give yogurt to a child who is severely allergic to milk. Instead, talk with your doctor about when/if yogurt could be introduced.
Targeted interventions based on your genes:
IL-10 and Leaky Gut
Studies show that people with IL-10 variants are more likely to have intestinal barrier function problems (e.g. leaky gut) when eating processed foods that contain emulsifiers and surfactants, such as polysorbate 80 and carboxymethylcellulose. If you have the IL-10 C allele highlighted below, read through the full article on leaky gut and emulsifiers.
Members: Your genotype for rs1800896 is —.
TLR6 variants: Farm life
The TLR6 gene encodes a pattern recognition receptor found on immune system cells. While not specific to milk allergies, a study showed that kids with TLR6 variants were more susceptible to allergies, and that growing up on a farm or in a rural environment mitigated the risk. Farm kids are exposed to a high microbial load of bacteria and fungi at a younger age.[ref]
FLG mutation and casein in skin care products:
The FLG mutations are strongly linked to atopic dermatitis and skin allergies — as well as food allergies. Research points to a link between sensitization dermally to an allergen and the development of food allergies.[ref] If you have the FLG mutation, avoiding milk products on your skin may be helpful. Casein is found in some skincare products such as anti-aging serums.[ref] Another skin exposure route is through soaps or shampoos that are “milk and honey” formulas or goat milk soap.[ref] Baby lotions sometimes contain milk or goat milk as well.
Related Articles and Topics: