Key takeaways:
~ Research indicates that CBD has anti-inflammatory, pain-relieving, and potential anti-anxiety and antidepressant effects.
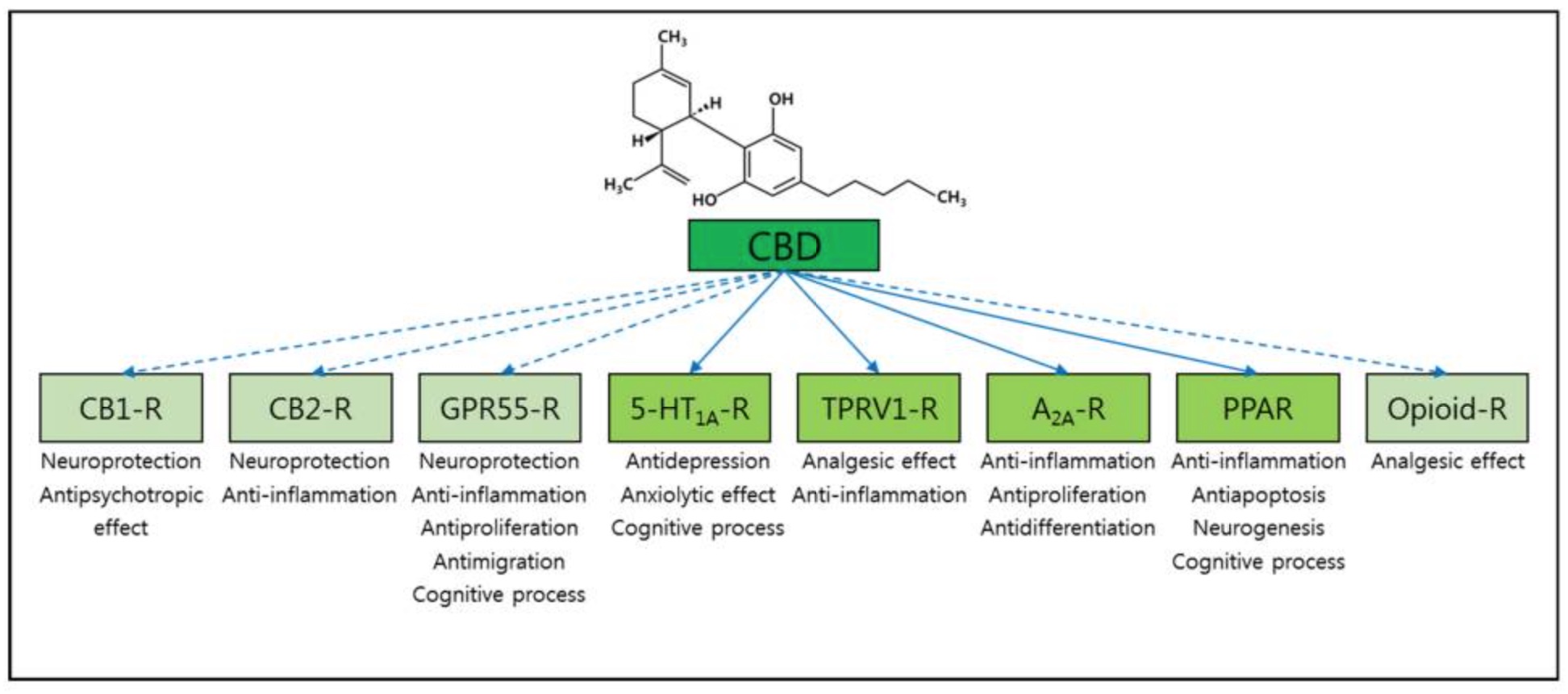
~ Unlike THC, which binds directly to cannabinoid receptors and causes psychoactive effects, CBD modulates various receptors, including serotonin, TRPV1 (pain), GPR55 (epilepsy), and adenosine receptors (sleep and inflammation).
~ Variants in these genes can change your response to CBD
Cannabidiol (CBD): Does It Work?
Cannabidiol, abbreviated CBD, is a phytocannabinoid found in cannabis (marijuana) and hemp plants. It was first isolated from the plant in the 1940s, and scientists unraveled its structure in the 1960s. It is a colorless solid at room temperature and is insoluble in water.
CBD does not cause psychoactivity (feeling high). Instead, it is being used for various anti-inflammatory and antiepileptic properties.[ref]
It is legal to buy cannabidiol oil in many places, but state laws can vary depending on whether the CBD is derived from hemp or cannabis. CBD derived from cannabis is often called ‘full spectrum’.
Cannabis research initially focused on THC, the psychoactive part of the plant, and the CBD component was pretty much ignored for many years. The past decade has seen an explosion of research on CBD, with several thousand studies referencing it now.
Interesting fact: Cannabis has been used for thousands of years. Researchers have analyzed cannabis found in a 2700-year-old grave of a shaman in China.[ref]
Your Endocannabinoid System
The psychoactive component of cannabis, Δ9-THC, binds to cannabinoid receptors in the body. These receptors are part of our endocannabinoid system. Cannabinoid receptors aren’t there just to bind to cannabis, of course. The endocannabinoid system regulates endocrine, immune, and brain functions. For example, it is involved in appetite control (why cannabis gives some people the ‘munchies’).[ref]
The body produces an endocannabinoid called anandamide, which is a lipid-based neurotransmitter. Anandamide binds to the cannabinoid receptors in the central and peripheral nervous systems. It plays a role in regulating mood, appetite, memory, sleep, temperature, and the development of an embryo.
But… CBD oil doesn’t really activate the cannabinoid receptors. Instead, it acts on several other receptors and modulates the response of the cannabinoid receptors.
Research Showing the Benefits of CBD Oil
Looking beyond the advertising hype, here is what research studies on CBD show:
Anti-inflammatory:
CBD is anti-inflammatory in the colon. A study used sections of inflamed colons from IBD, appendicitis, and bowel cancer patients to test the effects of CBD. The study found that CBD acts as an anti-inflammatory and prevents an increase in cytokine production in inflamed colon cells. It did not affect cancer cells in this study.[ref]
Pain:
CBD has been shown in animal studies to reduce pain. It may go along with the anti-inflammatory properties or may act through a different mechanism.[ref] CBD has also been shown to affect pain and inflammation when applied topically.[ref]
Addiction:
Animal studies have indicated that CBD might change behavior in heroin addiction. More research is needed on this, but CBD may be something to add to addiction rehab programs. [ref]
Intestinal Barrier:
Studies show that CBD can improve intestinal barrier function (reduce leaky gut!) for people with C. difficile infection.[ref]
Anxiety and Depression:
Several animal studies show that CBD may effectively relieve some symptoms of anxiety. A case study of a child with PTSD and sleep problems found that CBD was safe and effective for reducing anxiety. (More research must be done to know the full effects on kids!) [ref][ref][ref]
Several animal and human studies have shown that CBD has an antidepressant effect on some people.[ref][ref]
Epilepsy:
Some specific types of epilepsy can be treated using CBD.[ref][ref][ref] A randomized controlled trial for Dravet syndrome found that cannabidiol reduced seizure frequency more than placebo, but there was also a higher rate of adverse events.[ref]
Apoptosis:
Research shows that CBD oil induces apoptosis (cell death) in cervical cancer cells.[ref]
Acne:
A cell culture study shows that CBD oil may effectively treat acne vulgaris.[ref]
Sleep:
A study involving 72 adults found that CBD helped sleep scores in about two-thirds of patients. The study participants all were dealing with anxiety, and anxiety scores also decreased for the majority of the participants.[ref]
Antimicrobial:
Cannabidiol has been shown in several studies to act against biofilms and be antimicrobial for Gram-positive bacteria. The research points to membrane disruption as the mechanism of action.[ref]
Peripheral neuropathy:
Topical cannabidiol for peripheral neuropathy was investigated in a clinical trial. The results showed: “There was a statistically significant reduction in intense pain, sharp pain, cold and itchy sensations in the CBD group when compared to the placebo group. No adverse events were reported in this study.”[ref]
Caution and Safety:
A cell study published in 2019 shows that CBD could cause DNA damage. DNA damage is never good. Of course, the study needs to be replicated, but it does raise some questions about CBD being entirely safe.[ref]
Most animal and human studies show CBD oil to be safe and well-tolerated (even at high doses of up to 1,500mg/day). There have been side effects shown, such as interactions with medications. It is easy to think – ‘oh, this is just something natural from a plant’ – but instead consider it as a medication regarding interactions with other meds you are taking.[ref][ref]
CBD receptors: How CBD Actually Works
Cannabidiol interacts with various receptors in the body — which explains the great variety of different conditions that it treats. Due to genetic variants in the receptors, these different receptors may also explain the differences in effect people see when using CBD oil.
A little background on receptors:
Receptors are made up of a protein complex. The ligand is the molecule that binds to the receptor and activates it (e.g., cannabidiol). The metaphor commonly used to describe receptors and ligands is a lock and a key.
The ligand binds to a binding site on the receptor and activates it – like a key fitting into a lock.
- A molecule that fits into the receptor but doesn’t activate it – blocks the keyhole – is referred to as an antagonist of the receptor.
- A molecule that fits in the keyhole and activates the receptor (but isn’t the normal ligand) is an agonist.
This lock and key concept can get a little more complex when a molecule can bind to part of a receptor and cause the natural ligand to be either more active or less active — this is called an allosteric modulator. A positive allosteric modulator causes the receptor to be more active.
CBD binds to a serotonin receptor:
Cannabidiol interacts with the serotonin receptor 5-HT1A. It may be why, for some people, CBD oil reduces depression.
There is some question as to whether CBD binds directory to the serotonin receptor or whether it acts as an allosteric modulator, enhancing the signal of endogenous serotonin. Most of the recent studies point to it being an allosteric modulator, binding to the receptor and modifying serotonin uptake.[ref]
Animal studies show that the effect on the serotonin receptor is not due to any effect from the cannabinoid receptor (CB1). One study showed that repeated CBD dosing for seven days “reduced nerve injury-induced anxiety-like behavior”. In other words, surgery was performed on the animals to produce nerve pain, and seven days of CBD decreased the nerve pain and anxiety from the pain. The interaction with the serotonin receptor was the cause of the anti-anxiety effects.[ref][ref][ref][ref]
Reducing nausea: While people commonly think of serotonin receptors in the context of neurotransmitters and depression, the body also has serotonin receptors in the gut. For people with cancer, chemotherapy often causes nausea. It is triggered by serotonin released in the small intestines. Cancer patients often use cannabis (with THC and CBD) to counteract nausea.
An animal study showed that CBD suppresses vomiting.[ref]
TRPV1 (Pain receptor): Activated by CBD
CBD also activates and desensitizes the vanilloid 1 receptor (TRPV1).
The TRPV1 receptor is involved in the regulation of body temperature and in sensing heat and pain. Temperatures over 109 degrees F activate the receptor. Capsaicin, the hot spice in chili peppers, and isothiocyanate, which causes the hotness of wasabi and mustard, also activate the TRPV1 receptor.
Desensitization of the receptor, such as through repeated exposure to capsaicin, decreases its activity (and pain, such as from neuropathy).[ref]
CBD only acts on the vanilloid receptor at certain dosages, and the dose effect is thought to be a U-shaped curve. High doses of CBD show no effects on TRPV1 receptors.[ref][ref]
Related article: Specialized Pro-resolving Mediators also interact with TRPV1
CBD binds to GPR55
The G-protein coupled receptor 55 (GPR55) is a receptor found in the central nervous system and the intestines, bone marrow, endothelial cells, and platelets.
GPR55 is similar to the cannabinoid receptors (CB1 and CB2) but differs structurally in a couple of ways. CBD is a GPR55 antagonist — it blocks the function of the receptor. GPR55 is involved in axon growth and the wiring of the brain.[ref]
It is thought that CBD’s benefit in treating epilepsy is due to blocking GPR55 and decreasing the excitation of certain neurons. A lot of research is still going on about this topic, but it is exciting to see how a natural substance can be used for children with epilepsy.[ref]
Adenosine 2A Receptor: CBD and ADORA2A
The adenosine 2A receptor is one of several different adenosine receptors in the body. Adenosine is a molecule in the body that does many different things, including being a part of ATP (adenosine triphosphate) and cellular energy.
Adenosine also acts in cellular signaling and is a neuromodulator that promotes sleep. Caffeine binds to the adenosine 2A receptor, causing people to feel more awake. Additionally, the adenosine 2A receptor is involved in the immune system and cancer immunomodulation.[ref]
CBD has been shown in several recent studies to bind to the adenosine 2A receptor. In cannabis use, CBD blunts cognitive impairment that Δ9-THC causes — through its effects on the adenosine 2A receptor.[ref]
An animal study of lung inflammation found that CBD decreased the effects of the pro-inflammatory cytokines (TNF and IL-6) and other inflammatory pathways. This study clearly showed that the anti-inflammatory effects of CBD were due to the adenosine 2A receptor.[ref][ref]
A study showed that injecting CBD into the hypothalamus increases adenosine levels in the brain.[ref] This may affect sleep… One trigger for needing sleep is the accumulation of adenosine in the brain. Increased adenosine has been shown to increase non-REM sleep while decreasing REM sleep.[ref]
A rat study of CBD oil at two different concentrations showed that the total amount of sleep increased while higher doses delayed the onset of REM sleep.[ref]
CBD has also been shown to protect against heart arrhythmia (ventricular). It was shown to be through the activation of the adenosine A1 receptor.[ref]
CBD and GABA
There is some evidence that CBD acts on the GABA receptors also. GABA is the inhibitory neurotransmitter that blocks neurons from firing. It keeps the neurons from being overexcited.
A study using magnetic resonance spectroscopy to measure glutamate and GABA levels in the brain showed some interesting results. The study compared 17 neurotypical men and 17 autistic men at baseline and after a single dose of 600mg of CBD oil. The CBD increased subcortical glutamate but decreased cortical glutamate in both groups. But the results for GABA showed significant differences between neurotypical and autistic men. The GABA levels in neurotypical men increased after CBD, but the opposite happened for autistic men, with a (statistically) significant decrease.[ref]
Related article: GABA Genes
Platelets, Arachidonic Acid Release, and CBD
Both CBD and THC stimulate the release of arachidonic acid in platelets. CBD is a more potent activator of arachidonic acid than THC. Arachidonic acid is a polyunsaturated fatty acid that can be part of the cell membrane. It is also used to synthesize anandamide, the endocannabinoid our body produces that binds to the cannabinoid receptor.[ref] The release of arachidonic acid may increase anandamide, thus creating some of the pleasant effects associated with CBD.
CBD Oil Genotype Report
There is a huge variation in how people feel when they take CBD oil — some people find it has little to no effect, while others swear by it for everything. The difference is likely to be due to genetic variants, the unique changes that make us all individuals.
Lifehacks:
Buying Good CBD Oil:
What kind of CBD to buy – and where??
Honestly, I am not an expert on this and don’t want to steer anyone wrong. My only advice is to go with a reputable company with reviews from real people (not MLM shills).
A new startup company, Flower & Tonic, does independent lab testing of CBD products off the shelf. You may want to check that out — I like the idea of independent reviews based on testing products purchased at retail stores.
Dosages of CBD for different mood disorders:
Related Articles and Topics:
HPA Axis Dysfunction: Understanding Cortisol and Genetic Interactions
References:
Aso, Ester, et al. “Adenosine A2A-Cannabinoid CB1 Receptor Heteromers in the Hippocampus: Cannabidiol Blunts Δ9-Tetrahydrocannabinol-Induced Cognitive Impairment.” Molecular Neurobiology, vol. 56, no. 8, Aug. 2019, pp. 5382–91. PubMed, https://doi.org/10.1007/s12035-018-1456-3.
Bergamaschi, Mateus Machado, et al. “Safety and Side Effects of Cannabidiol, a Cannabis Sativa Constituent.” Current Drug Safety, vol. 6, no. 4, Sept. 2011, pp. 237–49. PubMed, https://doi.org/10.2174/157488611798280924.
Binder, Andreas, et al. “Transient Receptor Potential Channel Polymorphisms Are Associated with the Somatosensory Function in Neuropathic Pain Patients.” PLoS ONE, vol. 6, no. 3, Mar. 2011, p. e17387. PubMed Central, https://doi.org/10.1371/journal.pone.0017387.
—. “Transient Receptor Potential Channel Polymorphisms Are Associated with the Somatosensory Function in Neuropathic Pain Patients.” PLoS ONE, vol. 6, no. 3, Mar. 2011, p. e17387. PubMed Central, https://doi.org/10.1371/journal.pone.0017387.
Blessing, Esther M., et al. “Cannabidiol as a Potential Treatment for Anxiety Disorders.” Neurotherapeutics, vol. 12, no. 4, Oct. 2015, pp. 825–36. PubMed Central, https://doi.org/10.1007/s13311-015-0387-1.
Booz, George W. “Cannabidiol as an Emergent Therapeutic Strategy for Lessening the Impact of Inflammation on Oxidative Stress.” Free Radical Biology & Medicine, vol. 51, no. 5, Sept. 2011, pp. 1054–61. PubMed Central, https://doi.org/10.1016/j.freeradbiomed.2011.01.007.
Burstein, Sumner. “Cannabidiol (CBD) and Its Analogs: A Review of Their Effects on Inflammation.” Bioorganic & Medicinal Chemistry, vol. 23, no. 7, Apr. 2015, pp. 1377–85. PubMed, https://doi.org/10.1016/j.bmc.2015.01.059.
—. “Cannabidiol (CBD) and Its Analogs: A Review of Their Effects on Inflammation.” Bioorganic & Medicinal Chemistry, vol. 23, no. 7, Apr. 2015, pp. 1377–85. PubMed, https://doi.org/10.1016/j.bmc.2015.01.059.
Campos, Alline C., et al. “Plastic and Neuroprotective Mechanisms Involved in the Therapeutic Effects of Cannabidiol in Psychiatric Disorders.” Frontiers in Pharmacology, vol. 8, May 2017, p. 269. PubMed Central, https://doi.org/10.3389/fphar.2017.00269.
—. “Plastic and Neuroprotective Mechanisms Involved in the Therapeutic Effects of Cannabidiol in Psychiatric Disorders.” Frontiers in Pharmacology, vol. 8, May 2017, p. 269. PubMed Central, https://doi.org/10.3389/fphar.2017.00269.
Cekic, Caglar, and Joel Linden. “Adenosine A2A Receptors Intrinsically Regulate CD8+ T Cells in the Tumor Microenvironment.” Cancer Research, vol. 74, no. 24, Dec. 2014, pp. 7239–49. PubMed Central, https://doi.org/10.1158/0008-5472.CAN-13-3581.
Chagas, Marcos Hortes N., et al. “Effects of Acute Systemic Administration of Cannabidiol on Sleep-Wake Cycle in Rats.” Journal of Psychopharmacology (Oxford, England), vol. 27, no. 3, Mar. 2013, pp. 312–16. PubMed, https://doi.org/10.1177/0269881112474524.
Cherif, Hosni, et al. “Role of GPR55 during Axon Growth and Target Innervation.” ENeuro, vol. 2, no. 5, Nov. 2015, p. ENEURO.0011-15.2015. PubMed Central, https://doi.org/10.1523/ENEURO.0011-15.2015.
Couch, Daniel G., et al. “Cannabidiol and Palmitoylethanolamide Are Anti-Inflammatory in the Acutely Inflamed Human Colon.” Clinical Science (London, England: 1979), vol. 131, no. 21, Nov. 2017, pp. 2611–26. PubMed, https://doi.org/10.1042/CS20171288.
Crippa, José Alexandre de Souza, et al. “Effects of Cannabidiol (CBD) on Regional Cerebral Blood Flow.” Neuropsychopharmacology: Official Publication of the American College of Neuropsychopharmacology, vol. 29, no. 2, Feb. 2004, pp. 417–26. PubMed, https://doi.org/10.1038/sj.npp.1300340.
De Gregorio, Danilo, et al. “Cannabidiol Modulates Serotonergic Transmission and Reverses Both Allodynia and Anxiety-like Behavior in a Model of Neuropathic Pain.” Pain, vol. 160, no. 1, Jan. 2019, pp. 136–50. PubMed Central, https://doi.org/10.1097/j.pain.0000000000001386.
—. “Cannabidiol Modulates Serotonergic Transmission and Reverses Both Allodynia and Anxiety-like Behavior in a Model of Neuropathic Pain.” Pain, vol. 160, no. 1, Jan. 2019, pp. 136–50. PubMed Central, https://doi.org/10.1097/j.pain.0000000000001386.
de Mello Schier, Alexandre R., et al. “Antidepressant-like and Anxiolytic-like Effects of Cannabidiol: A Chemical Compound of Cannabis Sativa.” CNS & Neurological Disorders Drug Targets, vol. 13, no. 6, 2014, pp. 953–60. PubMed, https://doi.org/10.2174/1871527313666140612114838.
Deering-Rice, Cassandra E., et al. “Characterization of Transient Receptor Potential Vanilloid-1 (TRPV1) Variant Activation by Coal Fly Ash Particles and Associations with Altered Transient Receptor Potential Ankyrin-1 (TRPA1) Expression and Asthma.” The Journal of Biological Chemistry, vol. 291, no. 48, Nov. 2016, pp. 24866–79. PubMed Central, https://doi.org/10.1074/jbc.M116.746156.
—. “Characterization of Transient Receptor Potential Vanilloid-1 (TRPV1) Variant Activation by Coal Fly Ash Particles and Associations with Altered Transient Receptor Potential Ankyrin-1 (TRPA1) Expression and Asthma.” The Journal of Biological Chemistry, vol. 291, no. 48, Nov. 2016, pp. 24866–79. PubMed Central, https://doi.org/10.1074/jbc.M116.746156.
Devinsky, Orrin, et al. “Cannabidiol: Pharmacology and Potential Therapeutic Role in Epilepsy and Other Neuropsychiatric Disorders.” Epilepsia, vol. 55, no. 6, June 2014, pp. 791–802. PubMed Central, https://doi.org/10.1111/epi.12631.
Gigli, Stefano, et al. “Cannabidiol Restores Intestinal Barrier Dysfunction and Inhibits the Apoptotic Process Induced by Clostridium Difficile Toxin A in Caco-2 Cells.” United European Gastroenterology Journal, vol. 5, no. 8, Dec. 2017, pp. 1108–15. PubMed, https://doi.org/10.1177/2050640617698622.
Gomes, Felipe V., et al. “The Anxiolytic-like Effects of Cannabidiol Injected into the Bed Nucleus of the Stria Terminalis Are Mediated by 5-HT1A Receptors.” Psychopharmacology, vol. 213, no. 2–3, Feb. 2011, pp. 465–73. PubMed, https://doi.org/10.1007/s00213-010-2036-z.
Gonca, Ersöz, and Faruk Darıcı. “The Effect of Cannabidiol on Ischemia/Reperfusion-Induced Ventricular Arrhythmias: The Role of Adenosine A1 Receptors.” Journal of Cardiovascular Pharmacology and Therapeutics, vol. 20, no. 1, Jan. 2015, pp. 76–83. PubMed, https://doi.org/10.1177/1074248414532013.
Hammell, D. C., et al. “Transdermal Cannabidiol Reduces Inflammation and Pain-Related Behaviours in a Rat Model of Arthritis.” European Journal of Pain (London, England), vol. 20, no. 6, July 2016, pp. 936–48. PubMed Central, https://doi.org/10.1002/ejp.818.
Iannotti, Fabio Arturo, et al. “Nonpsychotropic Plant Cannabinoids, Cannabidivarin (CBDV) and Cannabidiol (CBD), Activate and Desensitize Transient Receptor Potential Vanilloid 1 (TRPV1) Channels in Vitro: Potential for the Treatment of Neuronal Hyperexcitability.” ACS Chemical Neuroscience, vol. 5, no. 11, Nov. 2014, pp. 1131–41. PubMed, https://doi.org/10.1021/cn5000524.
Iffland, Kerstin, and Franjo Grotenhermen. “An Update on Safety and Side Effects of Cannabidiol: A Review of Clinical Data and Relevant Animal Studies.” Cannabis and Cannabinoid Research, vol. 2, no. 1, June 2017, pp. 139–54. PubMed Central, https://doi.org/10.1089/can.2016.0034.
Kaplan, Joshua S., et al. “Cannabidiol Attenuates Seizures and Social Deficits in a Mouse Model of Dravet Syndrome.” Proceedings of the National Academy of Sciences, vol. 114, no. 42, Oct. 2017, pp. 11229–34. www.pnas.org, https://doi.org/10.1073/pnas.1711351114.
—. “Cannabidiol Attenuates Seizures and Social Deficits in a Mouse Model of Dravet Syndrome.” Proceedings of the National Academy of Sciences, vol. 114, no. 42, Oct. 2017, pp. 11229–34. www.pnas.org, https://doi.org/10.1073/pnas.1711351114.
Lukhele, Sindiswa T., and Lesetja R. Motadi. “Cannabidiol Rather than Cannabis Sativa Extracts Inhibit Cell Growth and Induce Apoptosis in Cervical Cancer Cells.” BMC Complementary and Alternative Medicine, vol. 16, no. 1, Sept. 2016, p. 335. PubMed Central, https://doi.org/10.1186/s12906-016-1280-0.
Mijangos-Moreno, Stephanie, et al. “Intrahypothalamic Injection of Cannabidiol Increases the Extracellular Levels of Adenosine in Nucleus Accumbens in Rats.” Neuroscience Research, vol. 84, July 2014, pp. 60–63. PubMed, https://doi.org/10.1016/j.neures.2014.04.006.
Oláh, Attila, et al. “Cannabidiol Exerts Sebostatic and Antiinflammatory Effects on Human Sebocytes.” The Journal of Clinical Investigation, vol. 124, no. 9, Sept. 2014, pp. 3713–24. PubMed Central, https://doi.org/10.1172/JCI64628.
Philpott, Holly T., et al. “Attenuation of Early Phase Inflammation by Cannabidiol Prevents Pain and Nerve Damage in Rat Osteoarthritis.” Pain, vol. 158, no. 12, Dec. 2017, pp. 2442–51. PubMed Central, https://doi.org/10.1097/j.pain.0000000000001052.
Pretzsch, Charlotte Marie, et al. “Effects of Cannabidiol on Brain Excitation and Inhibition Systems; a Randomised Placebo-Controlled Single Dose Trial during Magnetic Resonance Spectroscopy in Adults with and without Autism Spectrum Disorder.” Neuropsychopharmacology: Official Publication of the American College of Neuropsychopharmacology, vol. 44, no. 8, July 2019, pp. 1398–405. PubMed, https://doi.org/10.1038/s41386-019-0333-8.
Ren, Yanhua, et al. “Cannabidiol, a Nonpsychotropic Component of Cannabis, Inhibits Cue-Induced Heroin Seeking and Normalizes Discrete Mesolimbic Neuronal Disturbances.” The Journal of Neuroscience: The Official Journal of the Society for Neuroscience, vol. 29, no. 47, Nov. 2009, pp. 14764–69. PubMed, https://doi.org/10.1523/JNEUROSCI.4291-09.2009.
Resstel, Leonardo B. M., et al. “Effects of Cannabidiol and Diazepam on Behavioral and Cardiovascular Responses Induced by Contextual Conditioned Fear in Rats.” Behavioural Brain Research, vol. 172, no. 2, Sept. 2006, pp. 294–98. PubMed, https://doi.org/10.1016/j.bbr.2006.05.016.
Rock, Erin M., et al. “Interaction between Non-Psychotropic Cannabinoids in Marihuana: Effect of Cannabigerol (CBG) on the Anti-Nausea or Anti-Emetic Effects of Cannabidiol (CBD) in Rats and Shrews.” Psychopharmacology, vol. 215, no. 3, June 2011, pp. 505–12. PubMed, https://doi.org/10.1007/s00213-010-2157-4.
Rosenberg, Evan C., et al. “Therapeutic Effects of Cannabinoids in Animal Models of Seizures, Epilepsy, Epileptogenesis, and Epilepsy-Related Neuroprotection.” Epilepsy & Behavior: E&B, vol. 70, no. Pt B, May 2017, pp. 319–27. PubMed, https://doi.org/10.1016/j.yebeh.2016.11.006.
Russo, Chiara, et al. “Low Doses of Widely Consumed Cannabinoids (Cannabidiol and Cannabidivarin) Cause DNA Damage and Chromosomal Aberrations in Human-Derived Cells.” Archives of Toxicology, vol. 93, no. 1, 2019, pp. 179–88. PubMed Central, https://doi.org/10.1007/s00204-018-2322-9.
Russo, Ethan B., et al. “Phytochemical and Genetic Analyses of Ancient Cannabis from Central Asia.” Journal of Experimental Botany, vol. 59, no. 15, Nov. 2008, pp. 4171–82. PubMed Central, https://doi.org/10.1093/jxb/ern260.
Shannon, Scott, and Janet Opila-Lehman. “Effectiveness of Cannabidiol Oil for Pediatric Anxiety and Insomnia as Part of Posttraumatic Stress Disorder: A Case Report.” The Permanente Journal, vol. 20, no. 4, 2016, pp. 16–005. PubMed, https://doi.org/10.7812/TPP/16-005.
THE BRAIN FROM TOP TO BOTTOM. https://thebrain.mcgill.ca/flash/a/a_11/a_11_m/a_11_m_cyc/a_11_m_cyc.html. Accessed 6 Jan. 2022.
Viudez-Martínez, Adrián, et al. “Cannabidiol Regulates the Expression of Hypothalamus-Pituitary-Adrenal Axis-Related Genes in Response to Acute Restraint Stress.” Journal of Psychopharmacology (Oxford, England), vol. 32, no. 12, Dec. 2018, pp. 1379–84. PubMed, https://doi.org/10.1177/0269881118805495.
Xiong, Yinyi, and Chae-Seok Lim. “Understanding the Modulatory Effects of Cannabidiol on Alzheimer’s Disease.” Brain Sciences, vol. 11, no. 9, Sept. 2021. www.ncbi.nlm.nih.gov, https://doi.org/10.3390/brainsci11091211.
Zanelati, TV, et al. “Antidepressant-like Effects of Cannabidiol in Mice: Possible Involvement of 5-HT1A Receptors.” British Journal of Pharmacology, vol. 159, no. 1, Jan. 2010, pp. 122–28. PubMed Central, https://doi.org/10.1111/j.1476-5381.2009.00521.x.

