Key takeaways:
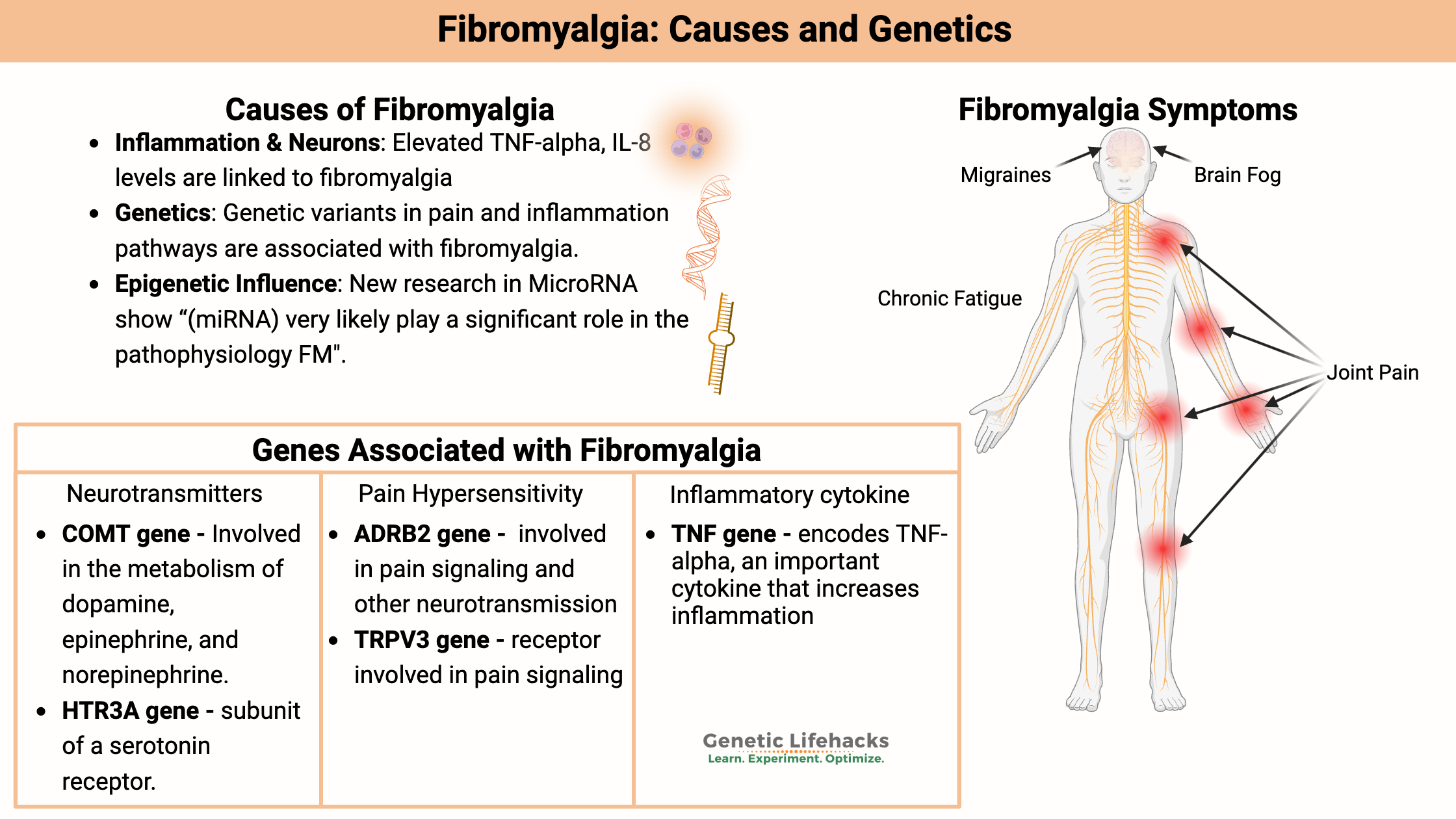
~ Fibromyalgia is a chronic pain syndrome involving widespread pain, fatigue, and cognitive issues (brain fog).
~ Inflammation and increased pain sensitivity due to altered nerve signaling may play a role in fibromyalgia symptoms.
~ Genetic and epigenetic factors, including microRNAs and mitochondrial dysfunction, contribute to the development of fibromyalgia.
~ Fibromyalgia often overlaps with other conditions, making accurate diagnosis essential. Understanding your genes can help you to sort out the right underlying cause.
What causes fibromyalgia?
Fibromyalgia is a chronic pain syndrome that causes generalized pain, fatigue, and overall general decline in function. It affects about 2-5% of the adult population.[ref][ref] According to the NIH health topic report on fibromyalgia, there is no cure, and scientists “do not fully understand what causes it”.[ref]
Other symptoms found in fibromyalgia:
According to the Mayo Clinic, in addition to widespread muscle and joint pain, people with fibromyalgia also often have fatigue, stiffness, sleep problems, brain fog, and mood issues. Comorbidities can include irritable bowel syndrome, ME/CFS, migraines, interstitial cystitis, TMJ, and POTS. [ref]
Diagnosing fibromyalgia:
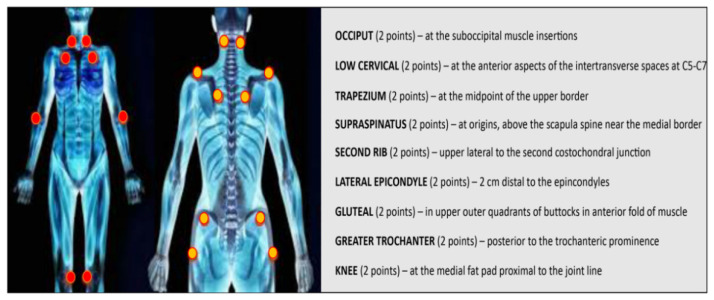
The American College of Rheumatology’s diagnostic criteria for fibromyalgia include central pain, above and below the waist, and pain on palpitation in 11 of 18 specific body sites (image below). The pain must last for more than three months.
The big question: What causes the pain in fibromyalgia?
This is a question that has puzzled doctors for some time. Let’s look at the research studies to see what is currently known about fibromyalgia and how genetic variants come into play. Then we will look at research studies and clinical trials on effective treatments for fibromyalgia and possible ways to reverse it.
Inflammation activates neurons:
One hypothesis of the root cause of fibromyalgia is elevated inflammatory cytokines, which are molecules released by immune system cells to cause inflammatory responses. The idea is that elevated inflammatory cytokines will cause the activation of nerve cells and thus cause pain.
Inflammatory cytokines:
Studies of fibromyalgia patients show mixed results, though, as to whether their inflammatory cytokine levels are elevated compared to healthy control groups. For example, some studies show that IL-8 is elevated while others don’t show statistical significance for inflammatory cytokines. One study, though, showed that even though TNF-alpha and IL-8 (inflammatory cytokines) levels were statistically in the same range as the healthy control group, the pain intensity was higher in fibromyalgia patients in accordance with higher TNF and IL-8 levels. IL-17 has also been shown to be elevated in fibromyalgia patients. Taken together, this suggests that neuroinflammation, perhaps at low levels, likely plays a role in the pathogenesis of fibromyalgia. [ref][ref][ref][ref]
NLRP3 inflammasome:
In addition to studies showing that higher levels of TNF and IL-8 are likely involved in fibromyalgia, studies have also shown that the NLRP3 inflammasome is activated.[ref] (This ties into the Lifehacks section and the clinical trials on supplements targeting NLRP3.)
Mast cells:
As part of the first line of defense against foreign pathogens and allergens, mast cells are often involved in increasing inflammation in certain tissues. Several studies and research papers explain that mast cell activation can lead to the inflammatory cytokines that activate pain receptors. For example, in addition to histamine, mast cells release TNF-alpha and other inflammatory mediators. Biopsies of fibromyalgia patients show increased numbers of mast cells. Mast cells are located in the areas that are the pain points in fibromyalgia [ref][ref][ref]
Hypersensitivity to pain:
The other side of the equation for people with fibromyalgia is that they seem to be more sensitive to pain. Feeling pain involves:[ref]
- stimulating nerve endings
- relaying that message to the brain
- modulation of that neural process to reduce the activity of the relayed message to the brain
- perception of the pain signal
Note that when research studies talk about hypersensitivity to pain, they don’t mean that the person with hypersensitivity is “just a pain wimp“. Instead, it indicates an alteration in the physiological detection of pain, often due to an increased number of receptors or increased transmission of pain.
Inflammation can be the initial stimulus for feeling pain, but the level at which nociceptors (pain receptors) are activated and the failure to reduce their activity to modulate pain appears to be altered in fibromyalgia.
Many of the genetic variants that increase the susceptibility to fibromyalgia are related to pain, with variants that increase sensitivity and neurotransmission being found more often in people diagnosed with fibromyalgia.
Genetic research on fibromyalgia:
A number of genetic variants are associated with an increased susceptibility to fibromyalgia, but a single gene doesn’t cause it. However, looking at the genetic pathways can shed light on the underlying cause for an individual. Genetic research is also important in helping researchers and doctors understand the biomarkers and body systems involved in fibromyalgia.
Many of the genetic variants that increase the relative risk of fibromyalgia are either related to overactivation of pain receptors (neurotransmitters, receptors for neurotransmitters, release of neurotransmitters) and/or increased activation of inflammation.[ref]
A preprint genome-wide association study in 2025 looked at genetic data from more than 2 million people, finding multiple genes that were associated with an increased risk of a diagnosis of fibromyalgia. Interestingly, the top hit was in the HTT gene, which is the gene that causes Huntington’s disease from rare mutations. Other notable genes identified included the dopamine receptor DRD2 and DCC, which is a gene that regulates myelin structure and axon organization for neurons.[ref]
MicroRNAs and gene expression:
Recent research is going beyond the gene variants that increase susceptibility to chronic diseases like fibromyalgia and looking at how gene expression is affected. There’s a lot of talk here at Genetic Lifehacks about the genes that code for proteins, but the segments of DNA that code for microRNA are also important.
MicroRNAs are non-coding RNA molecules (they don’t code for a protein) that can alter the regulation of protein expression and function. They are small segments of RNA that can control gene expression after it has been translated from DNA. Studies now show that miRNAs “very likely play a significant role in the pathophysiology of not only FM but also chronic pain”. Quite a few miRNAs have been found to be either downregulated or upregulated in fibromyalgia patients, either through serum testing or biopsies[ref][ref]
Mitochondrial genes:
A 2020 study looked at mitochondrial DNA (mtDNA) as a possible reason for fibromyalgia. The researchers found that one variant in a mitochondrial gene (not in 23andMe or AncestryDNA) that lowers mitochondrial membrane potential when oxidative phosphorylation is required was associated with susceptibility to fibromyalgia.
Mitochondria are the organelles that produce ATP, which cells use for energy. The mitochondrial membrane potential is part of the way that energy is converted in the mitochondria and used to make ATP. Essentially, it’s an electrochemical gradient across the inner mitochondrial membrane. Decreased mitochondrial membrane potential means that mitochondrial energy will be limited and cells that require a lot of energy (e.g. muscles) will rely more on glycolysis.[ref][ref] Animal studies on pain show that mitochondrial function in neurons is an important part of how chronic pain develops.[ref] You’ll see in the Lifehacks section that clinical trials show some efficacy for CoQ10 in fibromyalgia.
Is it fibromyalgia — or is it something else?
Fibromyalgia shares symptoms with a number of other conditions, and understanding these other conditions may help you narrow down whether you have the right diagnosis. Here are some conditions that are often mistaken for fibromyalgia due to overlapping symptoms, such as chronic pain, fatigue, and cognitive issues:
Small fiber neuropathy:
- Overlapping Symptoms: Small fiber neuropathy can cause chronic pain and sensitivity to touch. While there are some differences between small fiber neuropathy and fibromyalgia, about 40-60% of people diagnosed with fibromyalgia meet the biopsy criteria for small fiber neuropathy.[ref]
- Genetic connection: Read more about genetics and small fiber neuropathy
Familial Mediterranean Fever (FMF)
- Overlapping Symptoms: FMF and fibromyalgia both involve recurrent episodes of pain, fatigue, and sometimes joint or muscle pain. This is very similar to the widespread pain in fibromyalgia. A fairly common misdiagnosis and/or overlap is seen between familial Mediterranean fever mutation carriers and fibromyalgia.
- Genetic connections: You can check your genes for familial Mediterranean fever mutations here (also below in the genotype report section)
ME/CFS or long Covid
- Overlapping Symptoms: Both fibromyalgia and ME/CFS (chronic fatigue syndrome) can involve severe fatigue, brain fog, and sleep disturbances. ME/CFS is characterized more by overwhelming fatigue after minimal physical or mental exertion (post-exertional malaise), while fibromyalgia is known more for widespread pain and tender points. Fatigue, joint pain, and lack of exercise tolerance also coincide with long Covid, with some researchers suggesting a diagnostic overlap between long Covid and fibromyalgia.[ref]
- Genetic connections: Genetic variants have been identified that increase susceptibility to ME/CFS
Rheumatoid Arthritis (RA)
- Overlapping Symptoms: Joint pain, stiffness, and fatigue are common to both conditions. The difference is that RA is an autoimmune disease that causes joint inflammation and damage to the joints. This is usually diagnosed with blood tests looking for elevated inflammatory markers and using imaging. Fibromyalgia doesn’t cause joint damage or joint inflammation.
- Genetic connections: Genetic variants can increase susceptibility to RA and can guide treatment.
Lupus
- Overlapping Symptoms: The fatigue, widespread pain, and cognitive issues in lupus can mimic fibromyalgia. Lupus is an autoimmune disease that can affect multiple organs. Specific blood tests, like ANA (antinuclear antibody), can help distinguish lupus from fibromyalgia.
- Genetic connections: Read about lupus and genetic susceptibility.
Hypothyroidism
- Overlapping Symptoms Fatigue, muscle aches, joint pain, and depression are common in both fibromyalgia and hypothyroidism. Blood tests measuring thyroid function (TSH, T3, T4 levels) can help to show if your symptoms are from hypothyroidism.
- Genetic connection: Read more about thyroid hormones, genetics, and variants that interact with hypothyroidism.
Multiple Sclerosis (MS)
- Overlapping Symptoms: Fatigue, pain, cognitive dysfunction, and tingling sensations in MS can resemble fibromyalgia, however, MRI scans and neurological exams are used to see if brain and spinal cord lesions are present to indicate MS.
- Genetic connections: Read more about MS and genetic variants linked to increased susceptibility.
Myofascial Pain Syndrome (MPS)
- Overlapping Symptoms Chronic muscle pain and tenderness in localized areas can resemble fibromyalgia. Myofascial pain syndrome involves trigger points in muscles, often leading to localized pain. Fibromyalgia, on the other hand, involves widespread pain.
Ankylosing Spondylitis
- Overlapping Symptoms: Chronic pain, stiffness, and fatigue are common to both conditions. Ankylosing spondylitis is an uncommon form of inflammatory arthritis primarily affecting the spine. Imaging tests can help to distinguish it from fibromyalgia.
- Genetic connections. Most people with ankylosing spondylitis have the HLA-B27 genotype. You can check your HLA-B27 gene here.
Chronic Lyme Disease
- Overlapping Symptoms: Joint pain, muscle aches, fatigue, and cognitive difficulties are the overlapping symptoms. Lyme disease is caused by a bacterial infection (tick bite) which can sometimes be determined by a blood test. If untreated, it can cause chronic symptoms similar to fibromyalgia.
- Genetic connections: Read about the genetic variants that increase susceptibility to chronic Lyme
Irritable Bowel Syndrome (IBS)
- Overlapping Symptoms: Fibromyalgia and IBS often coexist, and both conditions involve abdominal discomfort and pain. IBS is primarily more of a digestive disorder that overlaps with fibromyalgia in the hypersensitivity to pain in the abdominal area.
- Genetic connections: Read about genetic variants related to IBS.
Ehlers-Danlos Syndrome or hypermobility spectrum disorder
- Overlapping symptoms: Chronic, widespread pain, fatigue, brain fog, and digestive issues are common in both fibromyalgia and EDS. The difference is that EDS often involves joined dislocations that aren’t usually seen in fibromyalgia. A study involving 63 fibromyalgia or ME/CFS patients found 81% met the criteria for hypermobility syndrome and 18% met the criteria for hEDS.[ref]
- Genetic connections: Read more about EDS and genetic mutations that cause it.
Genotype report: Fibromyalgia
Access this content:
An active subscription is required to access this content.
Lifehacks:
Fibromyalgia can be an overwhelming diagnosis, in part because of the frustrating lack of good information on ways to treat it or even reverse it.
I’m going to go through some of the clinical trials and research studies on the non-pharmaceutical options for fibromyalgia. Please be sure to talk to your doctor if you have any medical questions about what is right for you.
Studies on Natural Supplements for Fibromyalgia:
Access this content:
An active subscription is required to access this content.
Related articles and topics:
Specialized Pro-resolving Mediators (SPMs): The Resolution of Inflammation
TNF-alpha: Inflammation, Chronic Diseases, and Genetic Susceptibility