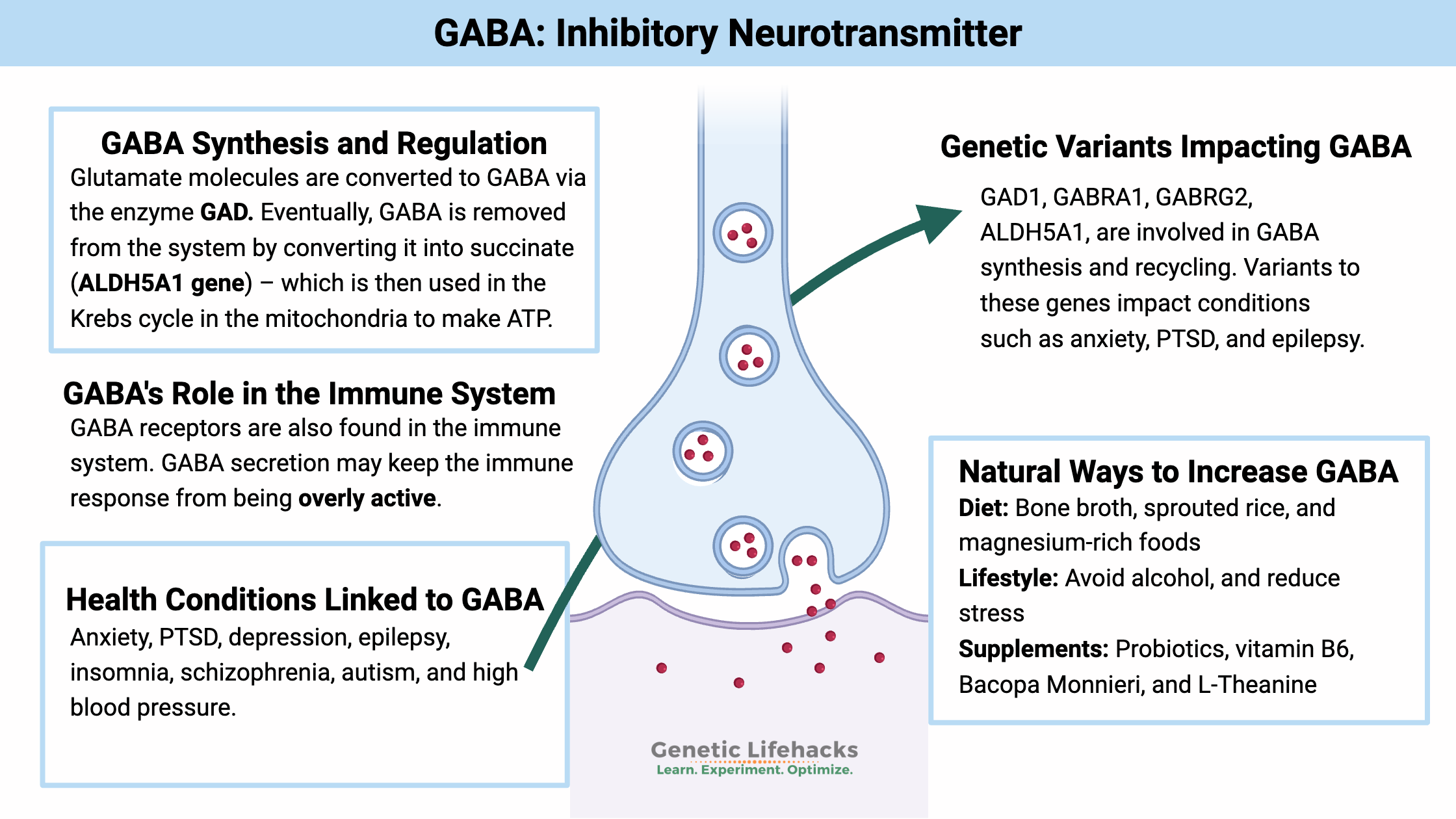
GABA (gamma-Aminobuyteric acid) is an inhibitory neurotransmitter that acts to stop a neuron from firing. This is an essential way that the brain regulates impulses. Low GABA levels are linked to anxiety and PTSD.
This article explains the role of GABA in the brain – including how neurons make GABA and the regulation of the amount of GABA inhibition in the brain. GABA also affects the immune system response, autoimmune diseases, and more.
We will dive into the genetic variants that can alter your GABA levels and then finish with natural ways to increase GABA. Members will see their genotype report below, plus additional solutions in the Lifehacks section. Join today.
What does GABA do?
I’m going to cover how GABA:
- gets created
- reuptake by receptors
- then broken down and recycled
But first, let me give you some background science on how neurons work as a context for the information on GABA in the brain. Skip ahead if you’re an expert here…
Neurons are nerve cells that communicate with another nerve cell by sending an electrical signal along the axon to the next neuron. Ions moving in or out of the cell cause a change in the electron balance, resulting in an electrical signal.
Excitation and firing:
Neurons can be excited and send a signal (fire) due to a stimulus.
Example: Neurons in the brain’s auditory cortex respond to the noises you hear.
But just as important as it is for a neuron to be excited and transmit a signal, it is also important for there to be a way to slow down or turn off that firing when needed. Using noise as an example, you need to filter out background sounds so you aren’t constantly bombarded.[ref]
Putting on the brakes with GABA:
Inhibiting or slowing down neurons is where the neurotransmitter GABA comes in.
About 20-25% of the neurons in the brain’s cortex are GABAnergic neurons. It means that they release GABA to inhibit other neurons from firing.
Below is a neuron and the synaptic terminals. Keep in mind that the neurons can interact with more than one neuron – it’s more like an intertwined network rather than just one neuron signaling one other neuron.
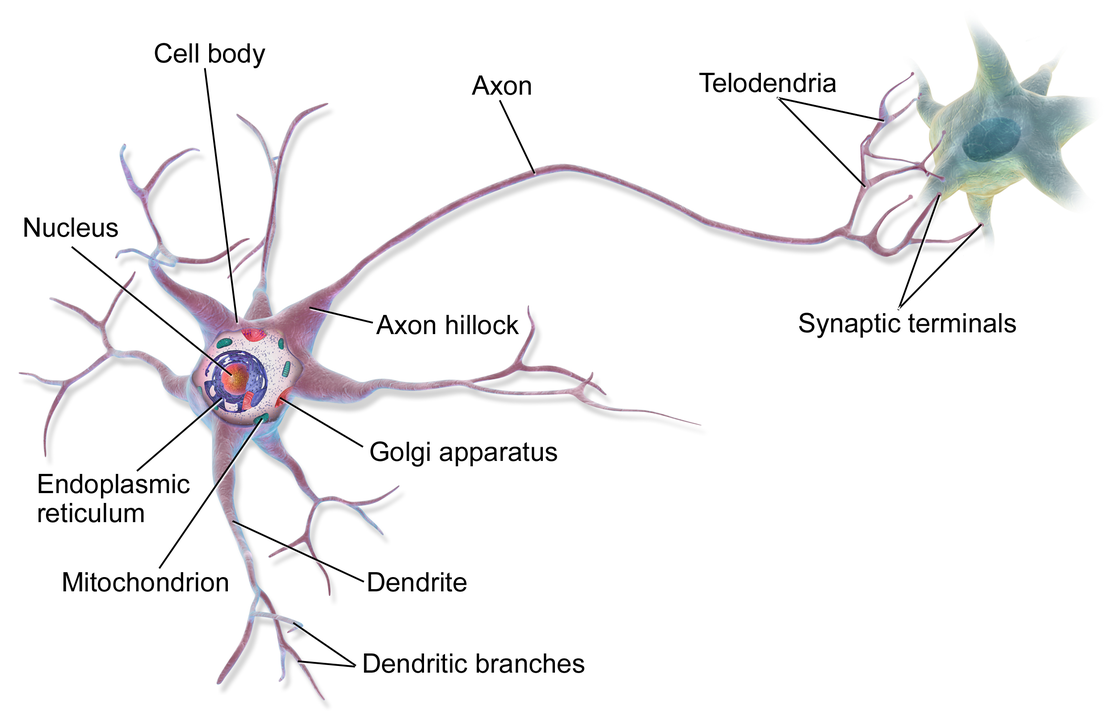
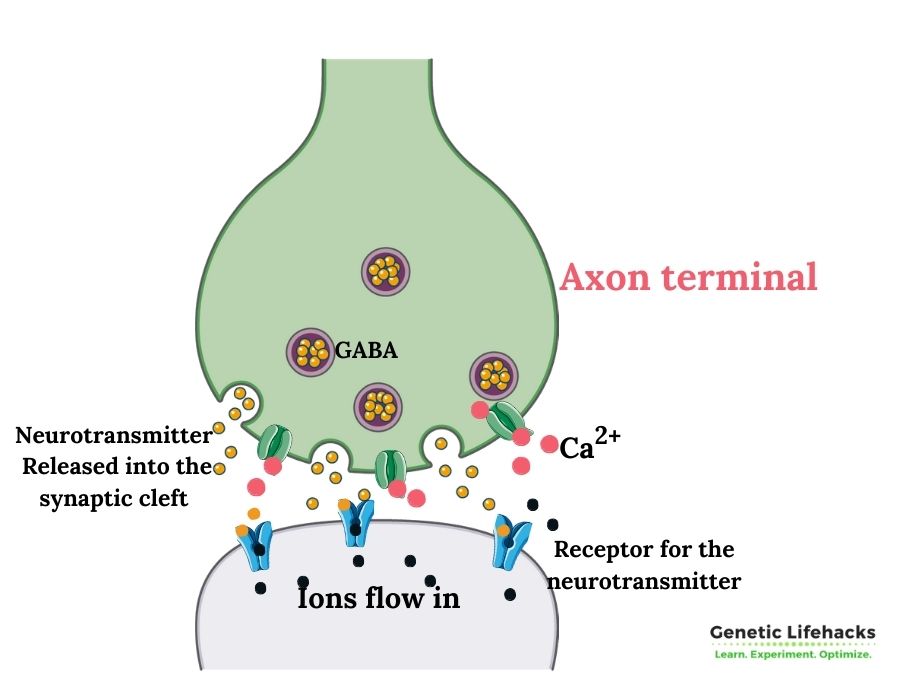
Within that synaptic terminal at the end of the axon, the electrical signal causes the release of a neurotransmitter.
Ions flowing, neurons firing:
Neurons fire by building up an action potential. It is all done by moving ions (e.g., calcium, potassium, chlorine) into or out of the cell, causing a change in the polarization – positive and negative charges – of the cell.
Ions and electrical charges:
Polarization happens when the electrical charges on the outside of the cell are positive, and the inside of the cell is negative. When the negative charge inside the cell reaches a certain voltage potential, the neuron ‘fires’, sending a signal down the axon to cause the release of a neurotransmitter into the synapse.
One way to inhibit a neuron from firing is to move chlorine ions into the cell or potassium ions out of a cell, decreasing the action potential.
It is what GABA does – it causes ions to move, changing the voltage potential within the cell.
Web of neurons:
Think of neurons as being like a net or a spider web, all interacting. Some neurons may release GABA to inhibit another neuron from firing – while other nearby neurons could send an excitatory signal simultaneously. It isn’t an all-or-nothing deal but a complex system of moving electrons.
Quick aside: GABA is not the only inhibitory neurotransmitter in the game. Glycine also works within the brain to inhibit excitation. Different parts of the brain have neurons inhibited by either glycine or GABA; thus, focusing on just one or the other may not give you the results you are looking for.[ref]
Recap: GABA is an inhibitory neurotransmitter that acts to decrease the stimulation of neurons.
Creation of GABA: Glutamate as a Precursor
GABA is usually created from glutamate, an amino acid, using the enzyme glutamic acid decarboxylase (GAD).
Two different forms of glutamic acid decarboxylase are coded for by the GAD1 and GAD2 genes.[ref]
What is Glutamate?
Glutamate is an amino acid that acts as an excitatory neurotransmitter, binding to its receptor and promoting the activation of neurons. Many people think of “MSG” and Chinese food when they hear the word glutamate, but glutamate occurs naturally throughout the body and is a vital neurotransmitter in the central nervous system.
As an excitatory neurotransmitter, glutamate is imperative for learning, attention, and focus – but too much glutamate causes too much stimulation in the brain. Balance is needed between stimulation and inhibition.
Where does the body get glutamate? Predominately from glucose. A precursor for glutamate called alpha-ketoglutarate is created in the mitochondria in the TCA cycle (Kreb’s cycle, producing ATP energy).
The alpha-ketoglutarate then converts to glutamate, which can be used as an excitatory neurotransmitter. Or, the glutamate can be further converted using the GAD1 enzyme and vitamin B6 into GABA.[ref]
Important point: The conversion of glutamate to GABA takes place in the GABAnergic neurons, which produce the GAD enzymes. Taking supplemental GABA likely does not cross the blood-brain barrier. Instead, GABA production occurs by utilizing glutamate in neurons.
Recap: GABA is created from glutamate using GAD1 or GAD2 enzymes with vitamin B6 as a cofactor.
GABA Receptors:
When released from the neuron, GABA needs to bind to a receptor on another nearby neuron to send its signal. Without a receptor, there is no action from GABA.
There are two types of GABA receptors: GABA-A and GABA-B
- GABA-A receptors are ionotropic Cl– (chloride ion) channels – allowing chloride to flow into a cell. It quickly changes the cell’s polarization, and the receptors are found in quick-acting neurons.
- GABA-B receptors are metabotropic, usually with potassium channels — causing potassium to flow out of the cell.
The GABA-A receptors (GABRA family of genes) are the most abundant and present throughout the central nervous system (brain, spinal cord). It is also found in immune cells and pancreatic beta-cells.
GABA-B receptors (GABRAB1 gene) are more specialized. They work to limit glutamate release and autoregulate the amount of GABA. When GABA binds to the GABA-B receptor, it is taken back into the neuron to be either recycled or broken down.[ref]
The third subtype of GABA receptor (GABA – C) impacts circadian rhythm, sleep, and the retina. It is referred to as GABA-C but is thought to be a subtype of GABA-A receptors.[ref][ref]
Breakdown of GABA:
Balanced: You don’t want too much GABA or too much glutamate at any one time. It’s a balance.
Eventually, GABA is removed from the system by converting it into succinate – which is then used in the Krebs cycle in the mitochondria to make ATP.[ref]
The enzyme succinic semialdehyde dehydrogenase (ALDH5A1 gene) is needed to convert GABA into succinate.[ref]
Rare genetic mutations in the ALDH5A1 gene cause succinic semialdehyde dehydrogenase deficiency, which decreases the breakdown of GABA. This results in increased brain levels of GABA. The increased amount of GABA then downregulates the GABA receptors, making the net effect less of an inhibitory signal.[ref]
GABA can also be metabolized into creatine, and an increase in both GABA and creatine is found in people with dysfunction in the ALDH5A1 gene.
GABA Transporters
The removal of GABA from the synapse occurs from the GABA transporter called GAT1 (SLC6A1 gene). It allows for the reuptake of GABA in the synapse. GAT1 also clears GABA from the extracellular space.
Animal studies show that knocking out the GAT1 gene causes spike-wave discharges in the brain. Rare GAT1 mutations can cause epilepsy.[ref]
GABA and Immune System Response
Much of what you read about GABA focuses on the brain and how GABA affects neurotransmitters, mood, and behavior.
However, GABA receptors are also found in the immune system, on T cells, as well as in macrophages, natural killer cells, mast cells, and dendritic cells. Activating the GABA-A receptor on T cells is thought to limit, or tamp down, CD8+ T cell response. Similarly, activating the GABA-A receptor on other immune system cells, such as mast cells, natural killer cells, macrophages, or dendritic cells, also inhibits their inflammatory activity.[ref][ref][ref][ref]
A question that puzzled researchers for a while was the source of GABA in the immune system. Recently, researchers found that B cells can synthesize and secrete GABA by producing the GAD1 enzyme.
B cell production of GABA may be an important way to modulate the immune response. For example, the interaction of GABA secreted by B cells may act to limit the CD8+ T cells in the vicinity. In this way, GABA secreted by B cells may keep the immune response from being overly active. It could be a benefit in situations with an overactive immune response, such as in sepsis or severe COVID-19. But it may be detrimental for killing cancer cells.[ref]
COVID-19: GABA may also help to limit an overactive immune response in severe COVID-19. Animal studies show that GABA receptor agonists effectively reduce mortality in a mouse model of Covid.[ref]
GABA and Autoimmune Diseases:
With the inhibitory effect of GABA on immune response, researchers are now looking at the possibility of using GABA or a GABA-receptor drug to modulate the immune response in autoimmune diseases.[ref]
Much of the research on GABA in the immune system and autoimmune diseases is very recent, with much of it only in animal models of diseases at this point.
- In a mouse multiple sclerosis (MS) model, a GABA-A receptor agonist, homotaurine, shows promise.[ref]
- Animal models of Sjögren’s syndrome show promise for using GABA to ameliorate symptoms. GABA administration increased tear and saliva production.[ref]
- Animal studies also show that GABA receptor activation can inhibit the development of rheumatoid arthritis.[ref]
- The brains of patients with MS were studied with MRIs. GABA and glutamate levels were significantly lower in the hippocampus when compared to a healthy control group. [ref]
Diabetes, pancreas, and GABA
In the pancreas, GABA is produced abundantly and is thought to regulate islet cell excitability and help regenerate beta-cells.[ref]
In type 1 and type 2 diabetes, there is a lack of GABA. Researchers have found that GABA helps to stabilize the insulin pulses in the beta-cells, with an overall effect of reducing insulin secretion. [ref]
Conditions linked to Altered GABA:
Altered GABA levels in the brain and central nervous system can lead to several different psychological disorders through either too much inhibition or not enough inhibition of neurons.
Anxiety disorders, PTSD:
As an inhibitory neurotransmitter, GABA puts the brakes on the release of neuropeptides in the brain that activate the hypothalamic-pituitary-adrenal (HPA) axis. The HPA axis controls stress hormone release, such as cortisol, from the adrenal glands. Some researchers think this interaction is a major player in anxiety disorders.[ref]
Related article: HPA axis genes.
Anxiety disorders like panic attacks, post-traumatic stress disorder (PTSD), or generalized anxiety disorder are characterized by low GABA levels in certain brain regions.[ref]
Additionally, people with an anxiety disorder may have overactivation in the amygdala caused by low GABA.[ref]
GABA is not the whole story! Anxiety (and depression) are complex disorders with many variables involved, so while GABA may play a role, anxiety disorders are likely multifactorial for most people. Read more about anxiety and genetics.
People with PTSD generally have lower brain GABA concentrations. Specifically, researchers found a reduction in GABA levels in the parieto-occipital cortex and the temporal cortex (regions in the brain). Glutamate levels showed increases compared to control in the temporal cortex.[ref]
Major Depressive Disorder:
Recurrent depression is a huge problem, with an estimated 1 in 5 people in the US dealing with depression.
For some people, GABA dysregulation may play a causal role in depression. In chronic stress conditions, a potassium-chloride transporter in the brain can be downregulated. It results in GABA being ineffective in inhibiting the HPA axis, leading to depression for some people.
Additionally, studies show that in acute psychological stress, GABA levels are decreased by 18% in the prefrontal cortex.[ref]
Studies also show that patients diagnosed with major depressive disorder have lower levels of GABA in the cortex than healthy controls. Interestingly, glutamate levels were the same between the patients and the control group.[ref]
Epilepsy:
Too much excitation in neurons in certain regions of the brain can cause epilepsy or spastic disorders.
Epilepsy is a complex topic, but essentially, an imbalance of GABA inhibition vs. excitation causes seizures. Many anticonvulsant drugs act by increasing GABA in the synapse.[ref]
Genetic variants that decrease the function of the GABA-A receptors – essentially decreasing GABA inhibition – are linked to an increased risk of epileptic seizures.[ref]
Insomnia:
Brain GABA levels were studied in people with primary insomnia who were not on medication. The results showed that people with long-term insomnia averaged 30% lower GABA levels in the brain than the normal sleeping control group.[ref]
Medications that block the GABA-B receptors (thus altering the recycling of GABA) alter sleep patterns and decrease slow-wave sleep. Animal studies also show that GABA-A antagonists injected into the brain cause a significant increase in REM sleep.[ref][ref] Learn more about slow-wave sleep.
Complex Interaction: It doesn’t seem to be as simple as ‘more GABA = better sleep’. Instead, drugs or supplements acting on GABA receptors may alter sleep structure (e.g., less slow-wave or more REM sleep).
Schizophrenia:
While there are still a lot of unknowns about schizophrenia, researchers theorize that this psychological disorder is due to a lack of GAD1 in certain regions of the brain.[ref] This lack of GAD1 theoretically leads to an imbalance of too much glutamate (excitation) and too little GABA (inhibition).
Autism:
Autism spectrum disorders are complex and heterogeneous. Some of the research on autism points to imbalanced glutamate and GABA neurotransmission.[ref][ref]
One thing to remember here is that GABA is an inhibitory neurotransmitter in the developed brain, but in the fetus or developing infant’s brain, GABA acts in different ways.
- A recent study found that in adults with autism, one portion of the brain had statistically decreased levels of glutamate, with GABA being the same as controls.[ref]
- Another study, though, found no differences in GABA or glutamate levels between young adults with autism and control in the brain regions examined.[ref]
- A recent study on the gut microbiome of children with ASD found a decrease in the abundance of gut bacteria that produce GABA.[ref]
High blood pressure:
Blood pressure control is a highly complex system in the body with many inputs.
- Animal models show that spontaneous hypertension can be due to reduced GABA inhibition in the part of the hypothalamus that regulates blood pressure. Animal studies found significantly fewer GABAnergic neurons in the hypothalamus.[ref]
- Further animal research points directly to an increase in GABA-B receptors, which clear out GABA from the synapse and shift towards less GABA available.[ref]
- Injecting GABA directly into the central nervous system (animal studies again) reduces blood pressure.[ref]
Circadian Rhythm and GABA:
The area of the brain known as the suprachiasmatic nucleus (SCN) is where the body’s core circadian clock is centered. The circadian clock plays an essential role in coordinating pretty much everything that goes on in the body – sleeping, waking, breaking down food, creating hormones at the right time, etc.
The type of neurons in the SCN is primarily GABAnergic, with over 90% of the neurons expressing GABA. While GABA is primarily an inhibitory neurotransmitter, the exception may be in the suprachiasmatic nucleus, where it seems that activation of the GABA-A receptor excites neurons. This depends on the flow of different ions, and the SCN neurons have a different balance of ion transporters.[ref][ref][ref]
Related article: Circadian rhythm genes
GABA Genotype Report:
Lifehacks for increasing GABA levels:
Many people look for ways to alter GABA levels when dealing with mood issues. Always keep in mind, though, that GABA is also acting on the immune system as well as the release of insulin in the pancreas.
Professional help:
If you are experiencing anxiety, depression, or another mood disorder, please see a doctor if you need medical help. While GABA may play a role, these complex disorders likely have multiple causes.
Dietary interventions:
Track to see if protein makes a difference:
What you eat can influence your brain’s neurochemistry to a degree. Glutamate is the precursor needed for the formation of GABA.
- A recent animal study showed that feeding rats a diet high in chicken or pork increased glutamate transporters and decreased GABA.[ref] This needs to be replicated in humans, but I include it so that you will be aware that specific foods may alter the balance of the glutamatergic system.
Keto:
A ketogenic diet enhances GABAnergic inhibition in the brain when used long-term. It is one way through which it helps with epilepsy.[ref] Some research points to the upregulation of certain GABA-producing bacteria in the gut as a mechanism of action for ketogenic diets to reduce epilepsy.[ref]
Bone Broth:
Glycine receptors are also inhibitory chloride channels – and there is cross-talk between glycine and GABA-A receptors.[ref] Glycine is abundant in bone broth and gelatin.
Alcohol:
At different levels, alcohol affects a couple of subtypes of GABA-A receptors.[ref] If you think you have GABA-related issues, try avoiding all alcohol for a while to see if you notice a change in your brain.
Sprouted rice:
Soaking and germinating brown rice increases the GABA content of the rice.[ref]
14 natural supplements that research shows will boost GABA:
Related Articles and Topics:
Dopamine Receptor SNPs: Addiction, Mood, ADHD, and Schizophrenia
COMT Gene: Neurotransmitter Levels, Estrogen Metabolism, and SNPs
References:
Ajram, L. A., et al. “Shifting Brain Inhibitory Balance and Connectivity of the Prefrontal Cortex of Adults with Autism Spectrum Disorder.” Translational Psychiatry, vol. 7, no. 5, May 2017, p. e1137. PubMed, https://doi.org/10.1038/tp.2017.104.
Averina, Olga V., et al. “The Bacterial Neurometabolic Signature of the Gut Microbiota of Young Children with Autism Spectrum Disorders.” Journal of Medical Microbiology, vol. 69, no. 4, Apr. 2020, pp. 558–71. PubMed, https://doi.org/10.1099/jmm.0.001178.
Belenky, Michael A., et al. “Heterogeneous Expression of Gamma-Aminobutyric Acid and Gamma-Aminobutyric Acid-Associated Receptors and Transporters in the Rat Suprachiasmatic Nucleus.” The Journal of Comparative Neurology, vol. 506, no. 4, Feb. 2008, pp. 708–32. PubMed, https://doi.org/10.1002/cne.21553.
Bhandage, Amol K., and Antonio Barragan. “GABAergic Signaling by Cells of the Immune System: More the Rule than the Exception.” Cellular and Molecular Life Sciences, vol. 78, no. 15, 2021, pp. 5667–79. PubMed Central, https://doi.org/10.1007/s00018-021-03881-z.
Brauns, Stefan, et al. “Genetic Variation in GAD1 Is Associated with Cortical Thickness in the Parahippocampal Gyrus.” Journal of Psychiatric Research, vol. 47, no. 7, July 2013, pp. 872–79. PubMed Central, https://doi.org/10.1016/j.jpsychires.2013.03.010.
Butilă, Anamaria Todoran, et al. “GABRG2 C588T Gene Polymorphisms Might Be a Predictive Genetic Marker of Febrile Seizures and Generalized Recurrent Seizures: A Case-Control Study in a Romanian Pediatric Population.” Archives of Medical Science : AMS, vol. 14, no. 1, Jan. 2018, pp. 157–66. PubMed Central, https://doi.org/10.5114/aoms.2016.63739.
CASTEL, MONA, and JOHN F. MORRIS. “Morphological Heterogeneity of the GABAergic Network in the Suprachiasmatic Nucleus, the Brain’s Circadian Pacemaker.” Journal of Anatomy, vol. 196, no. Pt 1, Jan. 2000, pp. 1–13. PubMed Central, https://doi.org/10.1046/j.1469-7580.2000.19610001.x.
de Leon, Anthony S., and Prasanna Tadi. “Biochemistry, Gamma Aminobutyric Acid.” StatPearls, StatPearls Publishing, 2022. PubMed, http://www.ncbi.nlm.nih.gov/books/NBK551683/.
Eggers, Erika D., and Peter D. Lukasiewicz. “GABA(A), GABA(C) and Glycine Receptor-Mediated Inhibition Differentially Affects Light-Evoked Signalling from Mouse Retinal Rod Bipolar Cells.” The Journal of Physiology, vol. 572, no. Pt 1, Apr. 2006, pp. 215–25. PubMed, https://doi.org/10.1113/jphysiol.2005.103648.
Fogaça, Manoela V., and Ronald S. Duman. “Cortical GABAergic Dysfunction in Stress and Depression: New Insights for Therapeutic Interventions.” Frontiers in Cellular Neuroscience, vol. 13, Mar. 2019, p. 87. PubMed Central, https://doi.org/10.3389/fncel.2019.00087.
GABA and Glycine. https://www.acnp.org/g4/GN401000008/Default.htm. Accessed 29 July 2022.
Gao, Fei, et al. “Altered Hippocampal GABA and Glutamate Levels and Uncoupling from Functional Connectivity in Multiple Sclerosis.” Hippocampus, vol. 28, no. 11, Nov. 2018, pp. 813–23. PubMed Central, https://doi.org/10.1002/hipo.23001.
Gauthier, P., et al. “Influence of a GABA(B) Receptor Antagonist on the Sleep-Waking Cycle in the Rat.” Brain Research, vol. 773, no. 1–2, Oct. 1997, pp. 8–14. PubMed, https://doi.org/10.1016/s0006-8993(97)00643-4.
Godfrey, Kate E. M., et al. “Differences in Excitatory and Inhibitory Neurotransmitter Levels between Depressed Patients and Healthy Controls: A Systematic Review and Meta-Analysis.” Journal of Psychiatric Research, vol. 105, Oct. 2018, pp. 33–44. PubMed, https://doi.org/10.1016/j.jpsychires.2018.08.015.
Gussin, Hélène A., et al. “Subunit-Specific Polyclonal Antibody Targeting Human Ρ1 GABA(C) Receptor.” Experimental Eye Research, vol. 93, no. 1, July 2011, pp. 59–64. PubMed, https://doi.org/10.1016/j.exer.2011.04.009.
Horder, Jamie, et al. “Glutamate and GABA in Autism Spectrum Disorder—a Translational Magnetic Resonance Spectroscopy Study in Man and Rodent Models.” Translational Psychiatry, vol. 8, May 2018, p. 106. PubMed Central, https://doi.org/10.1038/s41398-018-0155-1.
Horn, E. M., et al. “Decrease in Glutamic Acid Decarboxylase Level in the Hypothalamus of Spontaneously Hypertensive Rats.” Journal of Hypertension, vol. 16, no. 5, May 1998, pp. 625–33. PubMed, https://doi.org/10.1097/00004872-199816050-00010.
Johannesen, Katrine M., et al. “Defining the Phenotypic Spectrum of SLC6A1 Mutations.” Epilepsia, vol. 59, no. 2, Feb. 2018, pp. 389–402. PubMed Central, https://doi.org/10.1111/epi.13986.
Kirby, Trevor, et al. “Post-Mortem Tissue Analyses in a Patient with Succinic Semialdehyde Dehydrogenase Deficiency (SSADHD). I. Metabolomic Outcomes.” Metabolic Brain Disease, vol. 35, no. 4, Apr. 2020, pp. 601–14. PubMed Central, https://doi.org/10.1007/s11011-020-00550-1.
Kolodny, Tamar, et al. “Concentrations of Cortical GABA and Glutamate in Young Adults With Autism Spectrum Disorder.” Autism Research : Official Journal of the International Society for Autism Research, vol. 13, no. 7, July 2020, pp. 1111–29. PubMed Central, https://doi.org/10.1002/aur.2300.
Li, De-Pei, et al. “Plasticity of Pre- and Postsynaptic GABAB Receptor Function in the Paraventricular Nucleus in Spontaneously Hypertensive Rats.” American Journal of Physiology – Heart and Circulatory Physiology, vol. 295, no. 2, Aug. 2008, pp. H807–15. PubMed Central, https://doi.org/10.1152/ajpheart.00259.2008.
Luscher, Bernhard, et al. “The GABAergic Deficit Hypothesis of Major Depressive Disorder.” Molecular Psychiatry, vol. 16, no. 4, Apr. 2011, pp. 383–406. PubMed Central, https://doi.org/10.1038/mp.2010.120.
Lydiard, R. Bruce. “The Role of GABA in Anxiety Disorders.” The Journal of Clinical Psychiatry, vol. 64 Suppl 3, 2003, pp. 21–27.
Ma, Pengju, et al. “Effect of GABA on Blood Pressure and Blood Dynamics of Anesthetic Rats.” International Journal of Clinical and Experimental Medicine, vol. 8, no. 8, Aug. 2015, pp. 14296–302. PubMed Central, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4613098/.
Malaspina, Patrizia, et al. “Comparative Genomics of Aldehyde Dehydrogenase 5a1 (Succinate Semialdehyde Dehydrogenase) and Accumulation of Gamma-Hydroxybutyrate Associated with Its Deficiency.” Human Genomics, vol. 3, no. 2, Jan. 2009, pp. 106–20. PubMed, https://doi.org/10.1186/1479-7364-3-2-106.
Marenco, Stefano, et al. “Genetic Modulation of GABA Levels in the Anterior Cingulate Cortex by GAD1 and COMT.” Neuropsychopharmacology, vol. 35, no. 8, July 2010, pp. 1708–17. PubMed Central, https://doi.org/10.1038/npp.2010.35.
McNeill, John K., et al. “Functional Significance of the Excitatory Effects of GABA in the Suprachiasmatic Nucleus.” Journal of Biological Rhythms, vol. 33, no. 4, Aug. 2018, pp. 376–87. PubMed Central, https://doi.org/10.1177/0748730418782820.
Menegaz, Danusa, et al. “Mechanism and Effects of Pulsatile GABA Secretion from Cytosolic Pools in the Human Beta Cell.” Nature Metabolism, vol. 1, no. 11, Nov. 2019, pp. 1110–26. PubMed Central, https://doi.org/10.1038/s42255-019-0135-7.
Meyerhoff, Dieter J., et al. “Cortical Gamma-Aminobutyric Acid and Glutamate in Posttraumatic Stress Disorder and Their Relationships to Self-Reported Sleep Quality.” Sleep, vol. 37, no. 5, May 2014, pp. 893–900. PubMed Central, https://doi.org/10.5665/sleep.3654.
Mitchell, Amanda C., et al. “Transcriptional Regulation of GAD1 GABA Synthesis Gene in
the Prefrontal Cortex of Subjects with Schizophrenia.” Schizophrenia Research, vol. 167, no. 0, Sept. 2015, pp. 28–34. PubMed Central, https://doi.org/10.1016/j.schres.2014.10.020.
Pollock, Michael S., and Ralph E. Mistlberger. “Rapid Eye Movement Sleep Induction by Microinjection of the GABA-A Antagonist Bicuculline into the Dorsal Subcoeruleus Area of the Rat.” Brain Research, vol. 962, no. 1–2, Feb. 2003, pp. 68–77. PubMed, https://doi.org/10.1016/s0006-8993(02)03956-2.
Purves, Dale, et al. “GABA and Glycine.” Neuroscience. 2nd Edition, 2001. www.ncbi.nlm.nih.gov, https://www.ncbi.nlm.nih.gov/books/NBK11084/.
Song, Min, et al. “GABA Administration Ameliorates Sjogren’s Syndrome in Two Different Mouse Models.” Biomedicines, vol. 10, no. 1, Jan. 2022, p. 129. PubMed Central, https://doi.org/10.3390/biomedicines10010129.
Tian, J., et al. “GABA(A) Receptors Mediate Inhibition of T Cell Responses.” Journal of Neuroimmunology, vol. 96, no. 1, Apr. 1999, pp. 21–28. PubMed, https://doi.org/10.1016/s0165-5728(98)00264-1.
Tian, Jide, Min Song, et al. “Homotaurine Limits the Spreading of T Cell Autoreactivity within the CNS and Ameliorates Disease in a Model of Multiple Sclerosis.” Scientific Reports, vol. 11, Mar. 2021, p. 5402. PubMed Central, https://doi.org/10.1038/s41598-021-84751-3.
Tian, Jide, Hoa Dang, et al. “γ-Aminobutyric Acid Regulates Both the Survival and Replication of Human β-Cells.” Diabetes, vol. 62, no. 11, Nov. 2013, pp. 3760–65. PubMed Central, https://doi.org/10.2337/db13-0931.
Treiman, D. M. “GABAergic Mechanisms in Epilepsy.” Epilepsia, vol. 42 Suppl 3, 2001, pp. 8–12. PubMed, https://doi.org/10.1046/j.1528-1157.2001.042suppl.3008.x.
Weber, Heike, et al. “Gender Differences in Associations of Glutamate Decarboxylase 1 Gene (GAD1) Variants with Panic Disorder.” PLOS ONE, vol. 7, no. 5, May 2012, p. e37651. PLoS Journals, https://doi.org/10.1371/journal.pone.0037651.
Winkelman, John W., et al. “Reduced Brain GABA in Primary Insomnia: Preliminary Data from 4T Proton Magnetic Resonance Spectroscopy (1H-MRS).” Sleep, vol. 31, no. 11, Nov. 2008, pp. 1499–506. PubMed, https://doi.org/10.1093/sleep/31.11.1499.
Zhang, Baihao, et al. “B Cell-Derived GABA Elicits IL-10+ Macrophages to Limit Anti-Tumour Immunity.” Nature, vol. 599, no. 7885, Nov. 2021, pp. 471–76. PubMed, https://doi.org/10.1038/s41586-021-04082-1.