Key takeaways:
~ Gallstones are solid deposits that form in the gallbladder or bile ducts, primarily composed of cholesterol, bile pigments, and calcium salts.
~Gallstones typically form due to an imbalance in bile composition, where cholesterol levels exceed the capacity of bile salts and phospholipids to keep it dissolved.
~ Genetic variants increase the risk of gallstone in multiple ways. Understanding where your susceptibility lies can help you to find your right path for prevention.
Gallstones:
Your gallbladder is a small organ (~4 inches long) located on the upper right side of your abdomen, behind the liver. It stores bile, which your liver produces to break down fat in the foods you eat.
Gallstones (also called cholelithiasis) are hard ‘stones’ made of hardened bile. The composition of the stones can be either cholesterol or calcium bilirubinate. Cholesterol stones, the most common type, are thought to be formed if there is a lot of cholesterol in the bile. When the bile becomes supersaturated with cholesterol, the cholesterol can no longer be soluble in micelles (think oil droplets in water).[ref]
It is estimated that 10 – 40% of the population has gallstones, which are more common in women than in men. About 700,000 people each year in the US have their gallbladders removed.[ref] That is a lot of people missing an organ…
Let’s dig into what happens to cause gallstones…
How gallstones form:
Gallstones are solid deposits that develop in the gallbladder or biliary ducts. They are primarily composed of cholesterol, bile pigments, and calcium salts, and they can be classified as cholesterol, pigmented, and mixed gallstones depending on their chemical composition.
Bile is a digestive fluid produced in the liver for breaking down fats from foods, and it is stored in the gallbladder until needed. Normally, bile contains cholesterol, bile salts, and phospholipids in balanced proportions.
After you eat a large amount of food containing fat and protein, a neuroenteropeptide hormone called cholecystokinin (CCK) is released in the intestines. CCK then binds to the CCK1 receptor (CCK-1R) on the muscle cells of the gallbladder wall, triggering contraction of the gallbladder. When the gallbladder contracts, it pushes bile into the intestines.[ref]
Here’s how the gallstone formation process goes:
Supersaturation of Bile:
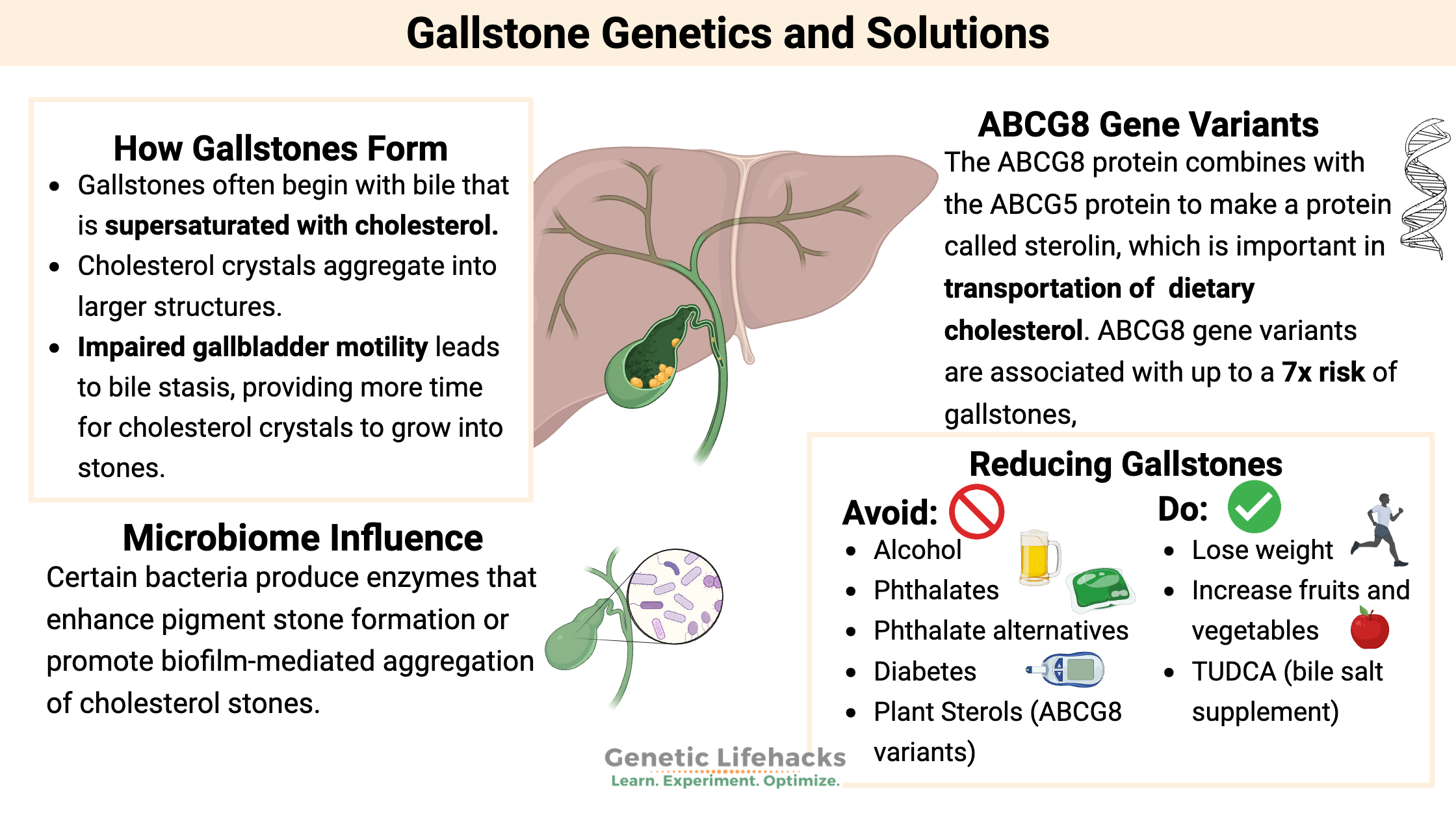
Gallstones often begin with bile that is supersaturated with cholesterol. When cholesterol levels exceed the capacity of bile salts and phospholipids to keep it dissolved, cholesterol crystallizes and forms the foundation for gallstones. The imbalance can come from too much cholesterol being produced or not enough bile acid being produced in the liver. Or it can be due to excess cholesterol absorption in the intestines.[ref]
Nucleation and crystals:
Mucins are glycoproteins secreted in the body to provide a thick, sticky, and protective layer, such as in the intestines, lungs, nose, and even the gallbladder.
Cholesterol crystals aggregate into larger structures when exposed to pronucleating factors, including mucin glycoproteins secreted by the gallbladder epithelium. Mucin acts as a scaffold for the formation of the gallstones.[ref]
Inflammatory changes in the gallbladder wall can further promote crystal growth by increasing mucin secretion.
Gallbladder Hypomotility:
Impaired gallbladder motility leads to bile stasis, providing more time for cholesterol crystals to grow into stones. Hypomotility can result from hormonal changes (e.g., pregnancy), rapid weight loss, or prolonged fasting.
Microbiome Influence:
Gut and biliary microbiota contribute to gallstone disease by altering bile composition and promoting biofilm formation around stones. Certain bacteria, such as Escherichia coli and Clostridium, produce enzymes like β-glucuronidase that enhance pigment stone formation or promote biofilm-mediated aggregation of cholesterol stones[ref][ref].
Gallstones Genotype Report:
Unsurprisingly, the genetic link to gallstones centers around the genes that regulate cholesterol absorption from plants and cholesterol excretion from the body.
Access this content:
An active subscription is required to access this content.
Lifehacks:
Plant Sterols:
Conflicting information exists for plant sterols from margarine or other foods labeled as “cholesterol-lowering plant sterols” in regards to gallstones and cardiovascular disease. The American Heart Association says plant sterols are good for reducing cardiovascular disease. But the ABCG8 variants that increase the risk of gallstones due to increased absorption of sterols also increase the risk of cardiovascular disease.
Related article: Plant sterols and your genes.
Estrogens (natural or environmental):
Environmental factors that increase gallstones include estrogens (women have more gallstones), oral contraceptives, and hormone replacement therapy.[ref]
Access this content:
An active subscription is required to access this content.
Related Articles and Topics:
LDL Cholesterol Genes
Your genes combine with your diet to influence your LDL cholesterol level. Learn more about why LDL cholesterol levels may matter in heart disease and find out how your genes are important here.
Heart disease, cancer, diabetes: A gene that ties together the “Big 3”
When it comes to chronic diseases, the “Big 3” are heart disease, cancer, and type 2 diabetes. Heart disease is the number one killer in the US, with cancer a close second. Diabetes numbers are increasing at an alarming rate.
Genetics and Type 2 Diabetes
Not all type 2 diabetes risk is from what you eat… Genetics plays a big role in diabetes. Learn more about your genetic susceptibility.
Inflammation: Causes and Natural Solutions
Take a deep dive into the causes of chronic inflammation and learn how to target specific inflammatory pathways to reverse or prevent chronic disease.
References:
Buch, Stephan, et al. “A Genome-Wide Association Scan Identifies the Hepatic Cholesterol Transporter ABCG8 as a Susceptibility Factor for Human Gallstone Disease.” Nature Genetics, vol. 39, no. 8, Aug. 2007, pp. 995–99. PubMed, https://doi.org/10.1038/ng2101.
Di Ciaula, Agostino, et al. “The Role of Diet in the Pathogenesis of Cholesterol Gallstones.” Current Medicinal Chemistry, vol. 26, no. 19, 2019, pp. 3620–38. PubMed, https://doi.org/10.2174/0929867324666170530080636.
Di Ciaula, Agostino, and Piero Portincasa. “Recent Advances in Understanding and Managing Cholesterol Gallstones.” F1000Research, vol. 7, Sept. 2018, p. F1000 Faculty Rev-1529. PubMed Central, https://doi.org/10.12688/f1000research.15505.1.
Frank, Kurtis, et al. Tauroursodeoxycholic Acid Research Analysis. Jan. 2022. examine.com, https://examine.com/supplements/tauroursodeoxycholic-acid/.
Goodloe, Robert, et al. “Lipid Trait-Associated Genetic Variation Is Associated with Gallstone Disease in the Diverse Third National Health and Nutrition Examination Survey (NHANES III).” BMC Medical Genetics, vol. 14, no. 1, Dec. 2013, p. 120. DOI.org (Crossref), https://doi.org/10.1186/1471-2350-14-120.
Joshi, Amit D., et al. “Four Susceptibility Loci for Gallstone Disease Identified in a Meta-Analysis of Genome-Wide Association Studies.” Gastroenterology, vol. 151, no. 2, Aug. 2016, pp. 351-363.e28. PubMed, https://doi.org/10.1053/j.gastro.2016.04.007.
Njeze, Gabriel E. “Gallstones.” Nigerian Journal of Surgery : Official Publication of the Nigerian Surgical Research Society, vol. 19, no. 2, 2013, pp. 49–55. PubMed Central, https://doi.org/10.4103/1117-6806.119236.
Paumgartner, G., et al. “Ursodeoxycholic Acid Treatment of Cholesterol Gallstone Disease.” Scandinavian Journal of Gastroenterology. Supplement, vol. 204, 1994, pp. 27–31. PubMed, https://doi.org/10.3109/00365529409103622.
Rodriguez, Santiago, et al. “Lipids, Obesity and Gallbladder Disease in Women: Insights from Genetic Studies Using the Cardiovascular Gene-Centric 50K SNP Array.” European Journal of Human Genetics, vol. 24, no. 1, Jan. 2016, pp. 106–12. PubMed Central, https://doi.org/10.1038/ejhg.2015.63.
Tsai, Chung-Jyi, et al. “Weight Cycling and Risk of Gallstone Disease in Men.” Archives of Internal Medicine, vol. 166, no. 21, Nov. 2006, pp. 2369–74. Silverchair, https://doi.org/10.1001/archinte.166.21.2369.
Wang, Siqi, et al. “Is the Oral Contraceptive or Hormone Replacement Therapy a Risk Factor for Cholelithiasis: A Systematic Review and Meta-Analysis.” Medicine, vol. 96, no. 14, Apr. 2017, p. e6556. PubMed, https://doi.org/10.1097/MD.0000000000006556.
Zhan, Lei, et al. “Prevalence of ABCB4 Polymorphisms in Gallstone Disease in Han-Chinese Population.” American Journal of Translational Research, vol. 8, no. 2, Feb. 2016, pp. 1218–27. PubMed Central, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4846965/.