Key takeaways:
~ Some people react to COVID-19 mRNA vaccines with side effects such as fever, fatigue, chills, and feeling unwell. While the CDC maintains that these side effects are normal, people’s reactions to the vaccine vary greatly – from no reaction to more severe reactions.
~Genetics is the other known factor in the immune system’s response to many different types of vaccination. (Read more: Vaccine Response and Your Genes)
Genetic variants and the COVID-19 vaccines:
We now have some information about genetic interactions with the Pfizer and Moderna mRNA vaccines for COVID-19. I’m sure more studies will come on this topic, but it is exciting to see the results from a large genetic-based study on the immune system’s response to side effects of the vaccine.
Let’s dig into the details of this study on genetics and the side effects of mRNA vaccines. (Currently, in preprint, read it for yourself):
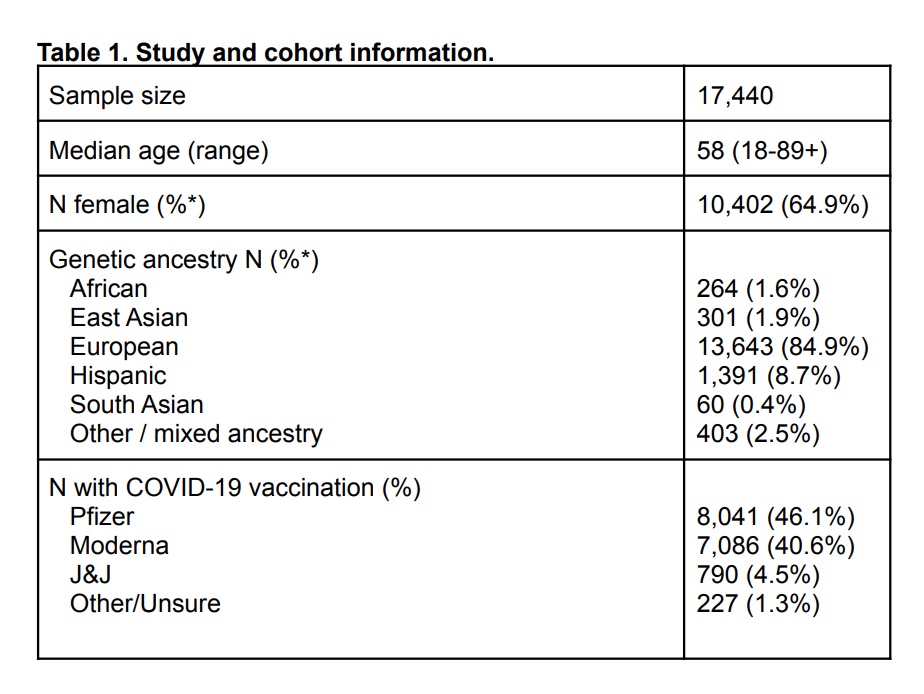
The study used survey information combined with DNA data from approximately 17,000 people in the US (mainly Nevada). The survey asked about previous COVID-19 infections before vaccination (7.3%)
Side effects reported:
The results of the vaccine reactions portion of the survey were as follows:
| Vaccine Reaction | % reporting |
|---|---|
| Extreme difficulties / unable to perform daily routine | 1,029 (8.0%) |
| Severe difficulties with daily routine | 1,237 (9.6%) |
| Moderate difficulties with daily routine | 2,597 (20.2%) |
| Mild difficulties with daily routine | 3,502 (27.2%) |
| No difficulties with daily routine | 4,500 (35.0%) |
In breaking down the results by manufacturer and by dose, the second dose of the Moderna shot had the most ‘severe or extreme’ reactions at 19.5%, with Johnson & Johnson coming in at 17.7% having a severe or extreme reaction.
While the study focused on the genetic variants linked with side effects, their results show that a prior COVID-19 infection was linked to greater side effects (which is what other studies and many anecdotes have shown). The <55 age group also had links to a greater risk of side effects, which makes sense with immune responses declining in aging.
Of note in this study is that the median age of participants was 58. Many participants may not have shown side effects due to an attenuated immune response in older individuals. Also important here, when it comes to the genetic part of the study, is that the vast majority of participants are of European or Hispanic ancestry. Thus, the genetic results may or may not hold true for other population groups.
Here is the participant breakdown:
HLA-A*0301 variant linked to mRNA side effects
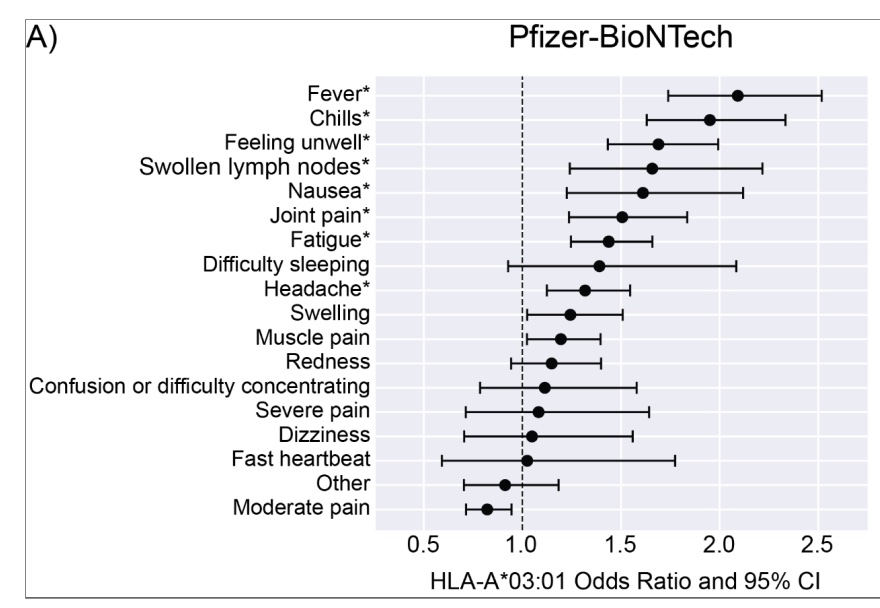
The researchers did a genome-wide association study, which looks across the whole genome to see if there is a statistical link to an outcome based on a genetic variant.
The results showed a sizable statistical link to a variant in the HLA-A gene. The HLA-A gene is also associated with an individual’s immune response to mumps, chickenpox, shingles, and other viruses.[ref]
Specifically, the side effects from the Pfizer vaccine were shown to be linked to HLA-A*0301, as shown in the image below. For example, people with this HLA type are twice as likely to have fever and chills and 1.5-fold more likely to have nausea, joint pain, and swollen lymph nodes.
mRNA Side Effects Genotype Report
Access this content:
An active subscription is required to access this content.
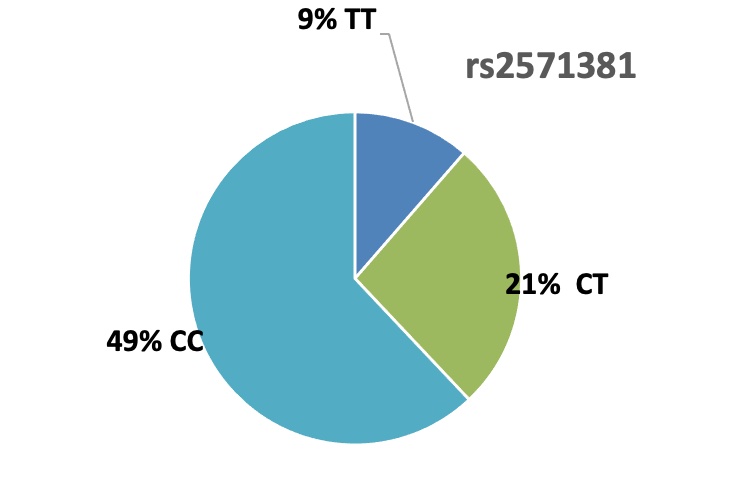
How common is this genotype? Almost a third of Caucasians carry this HLA type. It varies a bit in other population groups.
Conclusion:
What can you do with this information?
To state the obvious, if you have the HLA-A*03:01 type, you may want to plan for time off if getting the Pfizer vaccine – especially after the second dose and if you are under age 55. With boosters now being required in many places to be ‘fully vaccinated’, it will be interesting to see if this same increase in risk holds true for the third shot.
This HLA type is only linked to side effects from the vaccine. As far as I can find, it has not been linked to the severity of reactions to the SARS-CoV-2 virus in any of the genetic studies on COVID severity.
Research studies have been announced investigating whether some people are genetically less likely to get SARS-CoV-2. HLA types will likely play a role in susceptibility, but we will have to wait for those studies to be published.
Access this content:
An active subscription is required to access this content.
Related Articles and Topics
Guillain-Barré Syndrome: Genetic Risk Factors and Known Triggers
References:
Bolze PhD , Alexandre. “HLA-A*03:01 Is Associated with Increased Risk of Fever, Chills, and More Severe Reaction to Pfizer-BioNTech COVID-19 Vaccination.” MedRxiv, Nov. 2021, https://www.medrxiv.org/content/10.1101/2021.11.16.21266408v2.full.pdf+html.
Tian, Chao, et al. “Genome-Wide Association and HLA Region Fine-Mapping Studies Identify Susceptibility Loci for Multiple Common Infections.” Nature Communications, vol. 8, no. 1, Sept. 2017, p. 599. www.nature.com, https://doi.org/10.1038/s41467-017-00257-5.