A question from a patron via Patreon prompted me to look into the link between genes and Gulf War Illness. I want to share my findings in case it helps other veterans dealing with the after effects of their service to our country during the Gulf War.
Gulf War Illness (GWI)
The Dept. of Veteran Affairs explains that they don’t use the term Gulf War Syndrome or Gulf War Illness because of the variety of medically unexplained symptoms. For simplicity here, I will use the term Gulf War Illness (GWI) because ‘chronic multisymptom illness that is medically unexplained’ is way too long and vague.
The VA does state that it “presumes certain chronic, unexplained symptoms existing for 6 months or more are related to Gulf War service without regard to cause.” It includes quite of list of illnesses, including chronic fatigue syndrome, fibromyalgia, functional gastrointestinal disorders (IBS, dyspepsia, and abdominal pain), and undiagnosed illnesses (“abnormal weight loss, fatigue, cardiovascular disease, muscle and joint pain, headache, menstrual disorders, neurological and psychological problems, skin conditions, respiratory disorders, and sleep disturbances.“). That is quite an eye-opening list of the breadth and depth of the problems faced by Gulf War veterans![ref]
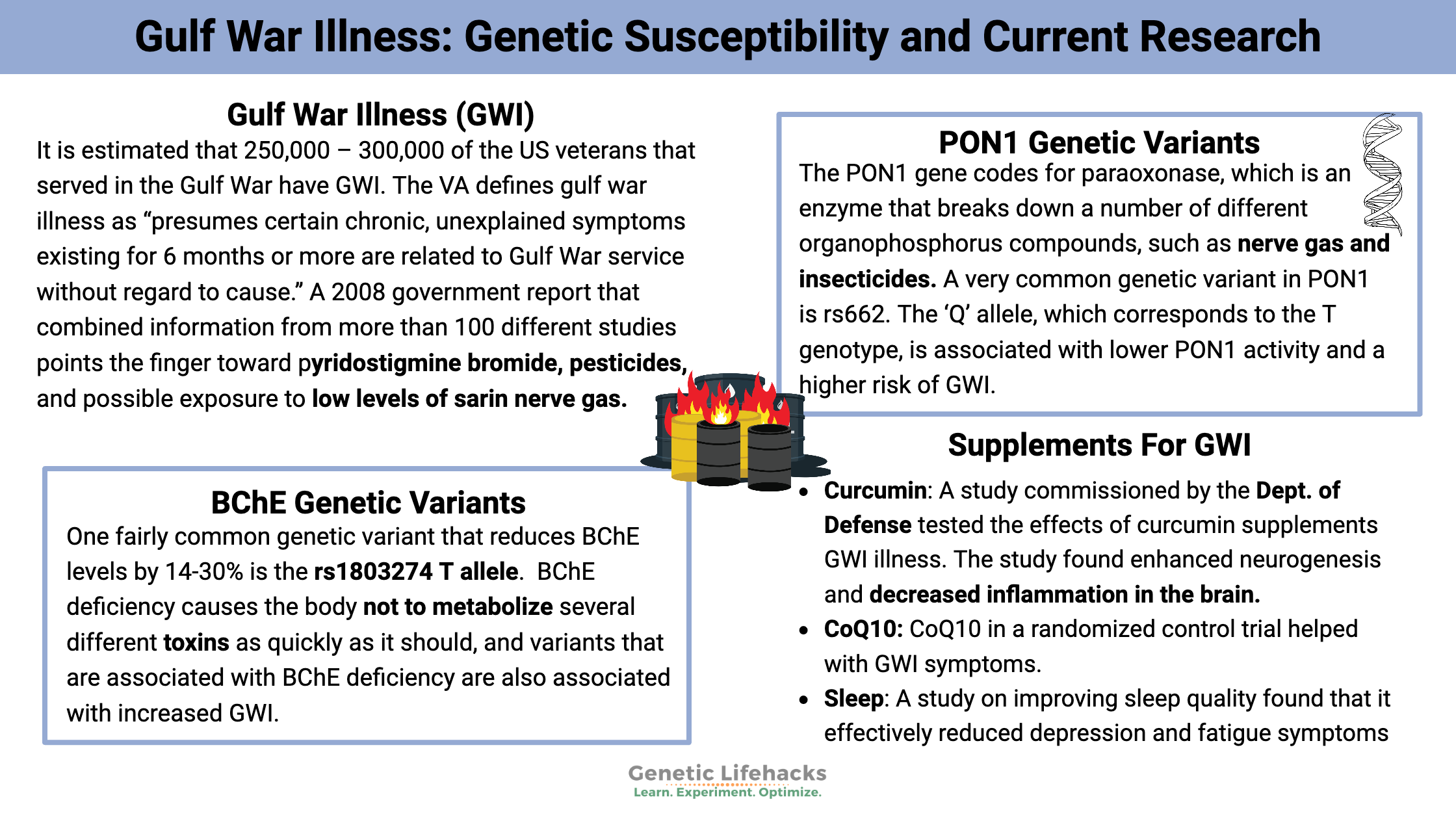
It is estimated that 250,000 – 300,000 of the US veterans that served in the Gulf War have GWI, and veterans from the UK were also affected. There were approximately 700,000 US troops involved in the Gulf War, so about 1/3 are affected in some way by chronic illnesses.[ref][ref]
Multiple theories have been proposed for the causal agent for GWI. Some of these theories include exposure to an infectious disease, exposure to biological or chemical weapons, vaccinations, depleted uranium exposure, and exposure to a variety of different chemical agents, including pyridostigmine bromide, organophosphate pesticides, decontamination agents, and petroleum exposure due to both fumes and oil well fire smoke.[ref]
As you can see, military personnel had exposure to multiple environmental toxins. It is entirely likely that there is not just one single cause of GWI, and exposure to one toxin could have led to increased susceptibility to another environmental agent.
A 2008 government report that combined information from more than 100 different studies points the finger toward pyridostigmine bromide, pesticides, and possible exposure to low levels of sarin nerve gas. You can read the full 465-page report.
I always find it interesting to look at how researchers create mouse or rat models of illnesses for their studies. For Gulf War Illness, researchers give mice pyridostigmine bromide (PB), DEET, and permethrin (a pyrethroid insecticide) and then stress the rats out for a period of time.[ref] PB is a preventative medication for sarin nerve gas exposure. The military personnel used insecticides, Deet, and permethrin.
The link between PB, pesticides, and sarin gas is all of these affect the body’s central nervous system through their effect on choline esterases. DEET not only affects the olfactory system of insects (mosquitoes dislike the smell of it), but it also inhibits cholinesterase activity in humans and strengthens the toxicity of another type of pesticide, carbamates.[ref] Permethrin uses commonly includes clothing and mosquito netting to kill insects, and it also kills lice.
So, how are genetics involved in all of this? Genes play a huge role in how our bodies react to environmental toxins. Some people are better than others at detoxifying different substances, including medications and toxins. (I have a whole bunch of articles on genetic variants involved in detoxification if you want more information on the topic.)
Gulf War Illness Genotype Report:
Not a member? Join here. Membership lets you see your data right in each article and also gives you access to the member’s only information in the Lifehacks sections.
BChE genetic variants:
The BCHE gene codes for the enzyme butyrylcholinesterase. It is mainly produced in the liver and found in blood plasma. A couple of variants of the gene can cause a deficiency in BChE. This BChE deficiency causes the body not to metabolize several different compounds as quickly as it should. Compounds metabolized by BChE include cocaine, heroin, and several anesthetics/nerve-blocking drugs (succinylcholine, mivacurium, and procaine). Additionally, BChE prevents organophosphate nerve agents (including sarin gas) and organophosphate insecticides from affecting the nervous system. People with genetic variants causing a decrease in the body’s production of BChE have a higher risk of being affected by organophosphates and of having adverse reactions to the anesthesia listed above.[ref]
Pyridostigmine bromide, which is an acetylcholinesterase inhibitor, was taken as a protective measure against nerve agents by about half of our military personnel in the Gulf War. One study found that personnel who took PB and were within a mile of an exploding SCUD missile (a stressor) were about 3 times more likely to have GWI. Veterans who had been in support areas and used personal pesticides also had an increased risk (12x) of GWI.[ref]
PB, as well as other acetylcholinesterase inhibitors, interact with both BChE and acetylcholinesterase (AChE). BChE is present in the blood at 10x the amount of AChE, and it protects people from having adverse reactions to carbamates and organophosphates (insecticides).[ref] (Note that there are virtually no AChE genetic variants affecting enzyme activity because it would cause embryonic lethality.)[ref]
One fairly common genetic variant that reduces BChE levels by 14-30% is the rs1803274 T allele. Studies refer to it as the K-variant. One study of GWI links it (along with other less active BChE variants) to up to a 40x increased risk of GWI. This is a huge increase in risk.[ref]
Check your genetic data for rs1803274 (23andMe v4, v5):
- T/T: K variant, ~14% reduction in BChE, increased risk of GWI[ref]
- C/T: carrier of one copy of the K variant, reduced BChE, increased risk of GWI
- C/C: typical
Members: Your genotype for rs1803274 is —.
Another variant found in about 1% of the population of the BChE gene is rs1799807. Having only about 40% of normal enzyme activity, studies call it the ‘atypical’ version of BChE.[ref] If you have the ‘atypical’ variant, you should tell your doctor this before having surgery, since it affects recovery from anesthetics.
Check your genetic data for rs1799807 (23andMe v4, v5; AncestryDNA):
- T/T: typical
- C/T: ‘atypical’ version of BChE, increased risk of GWI
- C/C: ‘atypical’ version of BChE, greatly increased risk of GWI
Members: Your genotype for rs1799807 is —.
Additionally, there are 20+ other mutations (all rare) that result in a significantly decreased BChE enzyme. These aren’t all covered in 23andMe data.[ref]
PON1 genetic variants:
Human susceptibility to adverse effects from organochloride pesticides (permethrin is one) is modified by the PON1 gene. The PON1 gene codes for paraoxonase, which is an enzyme that breaks down a number of different organophosphorus compounds, such as nerve gas and insecticides. It also is the enzyme that protects LDL cholesterol from oxidation (oxidized cholesterol is thought to be the cause of atherosclerosis, the hardening of the arteries). The PON1 gene modifies human susceptibility to adverse effects from organochloride pesticides (permethrin is one).
A very common genetic variant in PON1 is rs662. The ‘Q’ allele, which corresponds to the T genotype, is associated with lower PON1 activity and a higher risk of GWI. (Note that the T/T genotype for rs662 is very common, with almost half of Caucasians carrying it.)[ref][ref]
Recent studies have also found that this PON1 variant increases the risk of cardiovascular disease due to PON1’s effect on HDL levels, especially in people exposed to pesticides (e.g., coffee harvesters, sheep farmers).[ref][ref] Links also exist between an increased risk of anxiety and depression and those exposed to organophosphorus pesticides.
The research on the PON1 rs662 variant is extensive in looking at its effect on cardiovascular disease – extensive and contradictory. The effects of the variant seem to be related to ethnicity and also to environmental exposures. Not only does current exposure to pesticides have an effect, but also prenatal pesticide exposure changes the DNA methylation patterns of the gene (epigenetically decreasing its function). So while you can look at your genetics here, also keep in mind that your mom’s exposure to pesticides before your birth may play a role as well.[ref][ref]
Check your genetic data for rs662 (23andMe v4, v5; AncestryDNA):
- T/T: possibly higher risk of GWI[ref]
- C/T: typical variant
- C/C: normal risk of GWI
Members: Your genotype for rs662 is —.
Another study on PON1 levels in Gulf War veterans found that the average PON1 activity was lower in all Gulf War veterans regardless of genotype when compared to Bosnian peacekeeping veterans or non-deployed military personnel.[ref]
HLA DRB*13:02 Genetic Variant, Autoimmunity, and Inflammation:
Some veterans show protection from brain atrophy in GWI, depending on whether they carry a specific HLA type.[ref][ref] This may explain part of the differences in the severity of symptoms.
So what is an HLA type? The HLA (human leukocyte antigen) system is part of our adaptive immune system, the part of our immune system that remembers previous exposure to pathogens or toxins. For example, the adaptive immune system ‘remembers’ that you have already had chickenpox, and it can very quickly attack and destroy the virus with repeated exposures.
More specifically, HLA is a really complex system that brings parts of a molecule to the surface of a cell to signal that the cell needs to be destroyed by the body’s killer T-cells. Back to the example of the chickenpox virus – if a cell gets re-infected by the virus, the HLA system brings a piece of the virus to the cell’s surface, signaling the immune system to destroy the entire cell, thus destroying the virus replicating inside of the cell. There are a bunch of different HLA types with a variety of different components that bring about a huge number of possible combinations to counteract foreign invaders of all types. People inherit different alleles of the different HLA types, and because this system is highly polymorphic, susceptibility varies to different types of invaders or to autoimmune diseases. Overall, for the human species, this is really important to survival so that no single disease wipes us all out.
There have been a couple of studies showing that veterans who carry one particular HLA type, HLA DRB1*13:02, are less likely to have brain atrophy due to Gulf War Illness. In looking at genetic data, rs4759997 links to having HLA DRB1*13:02.[ref] 23andMe and Ancestry data do not contain this “rs” number at this time.
So, why include information on the rs id if it isn’t included in the common sources of genetic data? The mechanism by which the HLA DRB1*13:02 allele is protective is probably through its ability to eliminate some of the antigens that are causing chronic, low-grade inflammation and possibly autoimmunity.
The link to an inflammatory and autoimmune component in Gulf War Illness is important because many autoimmune conditions can be helped through diet.
Beyond the HLA DRB1*13:02 link to autoimmunity, there are other studies that indicate a possible immune system involvement in GWI. One (small) study found that veterans with GW had greater levels of inflammatory cytokines (IL-1B and IL-15) on days with higher fatigue severity.[ref] A larger study found the elevation of several different inflammatory proteins in veterans with GWI.[ref]
A recent study using a rat model of GWI (PB, pesticides, and 4 weeks of stress) shows a final link to immune system response. The study found that quite a few genes related to oxidative stress, antioxidant activity, neuroinflammation, and mitochondrial respiration were all upregulated, which means that all of those systems were activated in response to the chemicals and stress. This study concludes: “These results imply that chronic oxidative stress, inflammation, and mitochondrial dysfunction in the hippocampus, and heightened systemic inflammation and oxidative stress likely underlie the persistent memory and mood dysfunction observed in GWI.”[ref]
Lifehacks:
I don’t think there is a magic pill (yet?) to cure Gulf War Illness. The supplements and diet recommendations below may provide some help in healing your body. The best bet may actually be to try all of them.
Supplements, Diet & Lifestyle changes:
Curcumin: A study commissioned by the Dept. of Defense used rats that were exposed to low doses of GWI-related chemicals to test the effects of curcumin supplements. The study found enhanced neurogenesis (growth of neurons in the brain) and decreased inflammation in the brain. The study also found a reduction in oxidative stress and an increase in mitochondrial function, all thought to increase mood and memory.[ref]
Curcumin is a natural substance found in turmeric, which is a spice used in making curries. The body does not absorb Turmeric well on its own, so curcumin supplements containing piperine have been developed, increasing the body’s ability to absorb and use curcumin. You can probably find curcumin at your local grocery store or online.
CoQ10: Tying into the effects discussed above on mitochondrial function, CoQ10 in a randomized control trial helped with GWI symptoms. The study, which ran for 3.5 months, found a 100mg dose to work the best.[ref] CoQ10 is a well-studied and readily available supplement. If you are interested in other ways to improve mitochondrial function, you may want to read Dave Asprey’s book Head Strong.
Resveratrol: A 2016 placebo-controlled clinical trial found resveratrol “reduced GWI symptom severity significantly more than placebo at both the lower and higher dosages” [ref]
Related article: Resveratrol: Studies, Genetic Interactions, and Bioavailability
Sleep: A study on improving sleep quality found that it effectively reduced depression and fatigue symptoms in Gulf War veterans.[ref] Mind-body bridging, which I hadn’t ever heard of before, is used in the study to improve sleep quality.[ref] Another research-backed method of improving sleep quality includes blocking blue light at night by wearing blue-blocking glasses for two hours before bed. (This is one ‘lifehack’ that works really well for me!)
Diet: Considering the possible autoimmune link, check into the Autoimmune Protocol diet. Here is a good article on it: http://www.saragottfriedmd.com/is-the-autoimmune-protocol-necessary/. There is no real downside to trying this diet, and several people that I know with autoimmune diseases swear by it.
Avoid DEET, permethrin, and insecticides in general. Nope, I don’t have a study on this specifically for GWI, but common sense says if exposure to these insecticides was part of the problem, then avoiding further exposure is probably warranted.
There are a few alternatives to DEET, such as picaridin and lemon eucalyptus. Especially avoid DEET combined with other insecticides that are carbamates.[ref]
Permethrin is a very commonly used pesticide. If you have a company coming out to treat your home for bugs each year, you should check to see what kind of chemicals they are spraying. In agriculture, it is mostly used on wheat, corn, and cotton. Consider going with organic foods and possibly organic cotton. I was surprised to find out how extremely common it is to have permethrin in the body. A new study came out recently showing permethrin in 90% of breast milk samples.[ref]
Stress: Another way to create a rat model of GWI is to expose them to 4 days of corticosterone (equivalent to the effect of cortisol in humans) before injecting them with a sarin nerve agent surrogate. Chronic stress can cause high cortisol levels. It is conjecture on my part, but lowering cortisol levels (if they are high) may also help with some of the symptoms of GWI. Yoga, mindfulness meditation, or ashwagandha root supplement may help lower your cortisol levels.[ref] (Read more about ashwagandha research) Along that same line of thought, a 2016 study of Gulf War veterans found that mindfulness-based stress reduction reduces pain, fatigue, and cognitive failures.[ref] There are lots of websites and videos on mindfulness, and there are several good phone apps as well.
Acupuncture: A Dept. of Defense-sponsored study looked at the effectiveness of acupuncture as a treatment for GWI. It found that acupuncture reduced pain and reduced physical disability.[ref]
NRF2 activators: One more suggestion (not based on any GWI-specific research) is to look at supplements that increase NRF2. Rat models of GWI show the involvement of the NRF2 pathway. In general, NRF2 is involved in the body’s antioxidant defense system; it activates glutathione S-transferase and NQO1. Curcumin boosts NRF2, as does sulforaphane from broccoli sprouts.[ref]
Related article: Sulforaphane, studies, bioactivation
Research to keep an eye on:
Reversing the neuronal effects:
A study from July 2017 looked at the effects of GWI on human neurons. It found that there were problems with microtubule acetylation, and they could reverse it with an HDAC6 inhibitor. So in a basic sense, some of the genes in the neurons are turned off in GWI, and with the HDAC6 inhibitor, they are able to return the genes to normal function. This is somewhat hopeful if researchers can use it in the brain rather than just in a petri dish. HDAC6 inhibitors are in human clinical trials now for cancer and a few other diseases.[ref]
Light therapy:
Another research avenue to investigate is the use of transcranial red/near-infrared LED light therapy. There are studies going on with GWI veterans for this type of treatment.[ref] If you are interested in investigating it, you may also want to search for photobiomodulation in addition to low-level laser therapy.
Inflammation and TBI:
A Nov. 2018 study, “The Multiple Hit Hypothesis for Gulf War Illness: Self-Reported Chemical/Biological Weapons Exposure and Mild Traumatic Brain Injury” links mild traumatic brain injury during the war to increased susceptibility to GWI. In the study group (n=125), 100% of those with mild TBI also had Gulf War Illness. There is new research coming out all the time on the long-term impacts of TBI, and this may be another path to explore on the road to health.
What didn’t work:
Doxycycline: A large VA trial of doxycycline for possible mycotoxin-related illness showed no benefits.[ref]
Mifepristone, a corticosteroid, didn’t show much of an effect on GWI, although it did boost visual learning a little.[ref]
Carnosine: A clinical trial of carnosine also showed little effect other than a possible effect on memory. “12 weeks of carnosine (1500 mg) may have beneficial cognitive effects in GWI. Fatigue, pain, hyperalgesia, activity and other outcomes were resistant to treatment.”[ref]
Final thought:
I want to thank all of our Gulf War veterans for their service to our country, and I hope that the information provided here will be a good starting point for finding relief from their symptoms. Please remember that I’m not a doctor, and everything here is just my summary of research studies on the topic. I am sure that I have left some (probably important) things out, and I’m hopeful that there is much more research coming out soon on the topic.
Related Articles and Topics:
Circadian Rhythms: Genes at the Core of Our Internal Clocks
Circadian rhythms are the natural biological rhythms that shape our biology. Most people know about the master clock in our brain that keeps us on a wake-sleep cycle over 24 hours. This is driven by our master ‘clock’ genes.
Chronic Inflammation & Autoimmune Risk – IL17
Inflammation seems to be blamed for everything from heart disease to mood disorders to obesity. But how does this somewhat nebulous idea of too much inflammation tie into our genes? It seems that some people have a more sensitive immune system and are more prone to inflammatory reactions.