Key takeaways:
~ Hidradenitis suppurativa (HS) is a chronic inflammatory skin disease that causes lesions involving blocked hair follicles and exaggerated immune responses.
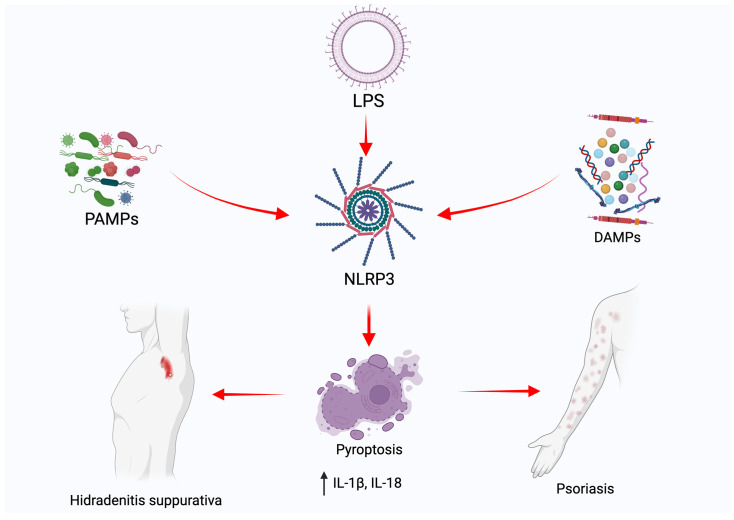
~ Elevated cytokines and activation of the NLRP3 inflammasome drive HS inflammation and pyroptosis (inflammatory cell death), which causes tissue damage.
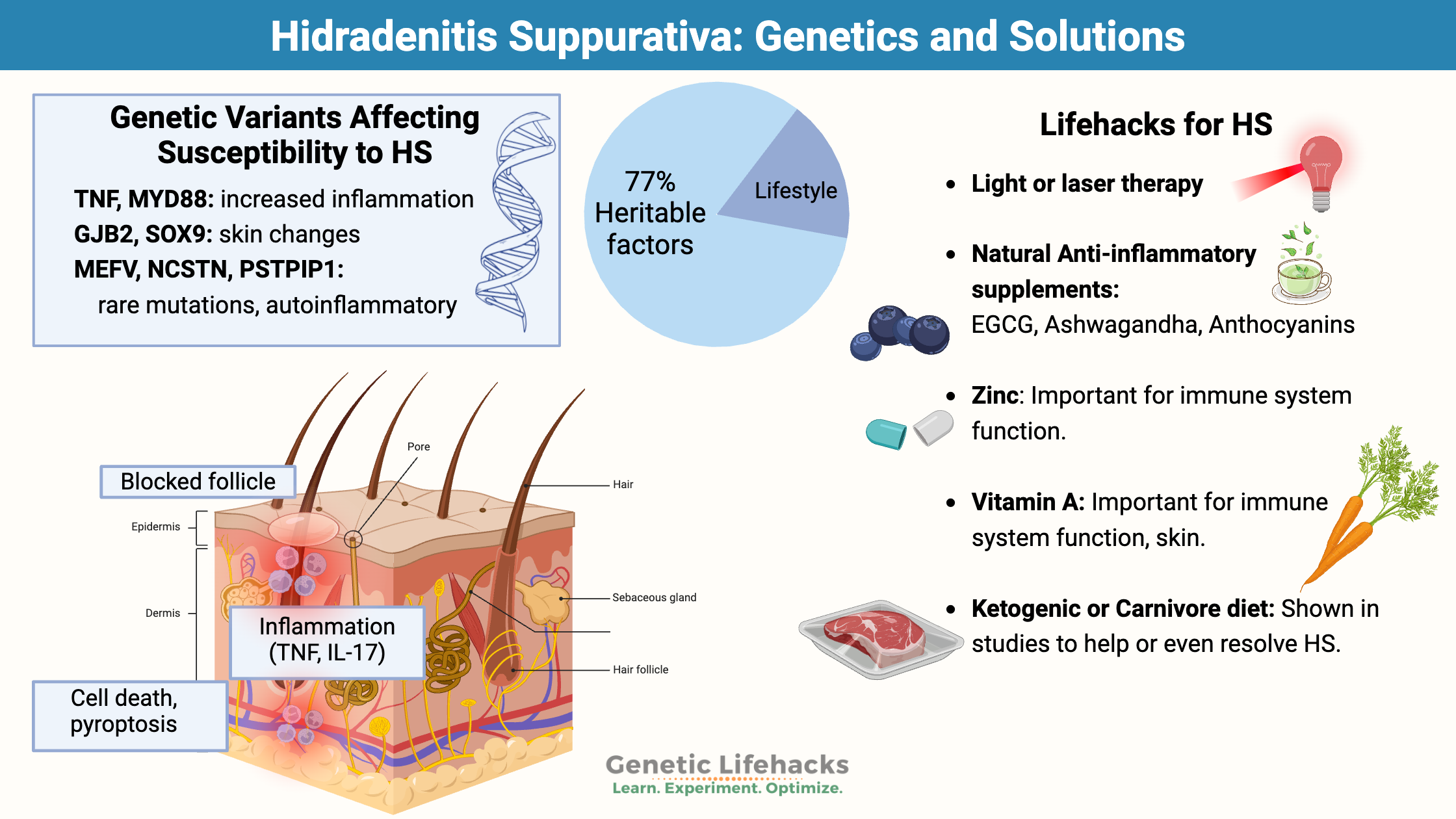
~ Genetic variants increase the susceptibility to HS, along with lifestyle and diet factors.
~ Understanding your genetic variants can help you know which treatments may work best for you.
Hidradenitis suppurativa and inflammatory cytokines:
Hidradenitis suppurativa (HS, or acne inversa) is an inflammatory skin disease that usually starts in young adulthood (20s – 30s). It’s more than just bad acne — painful nodules, abscesses, scarring, and what are called sinus tracts or fistulas, which are tunnels running back into the body.[ref]
HS affects the areas of the body that contain apocrine glands (armpits, groin, and around the nipple) and the perianal area. Researchers say that it causes a “negative impact on the quality of life” due to the painful lesions that secrete malodorous pus.[ref]
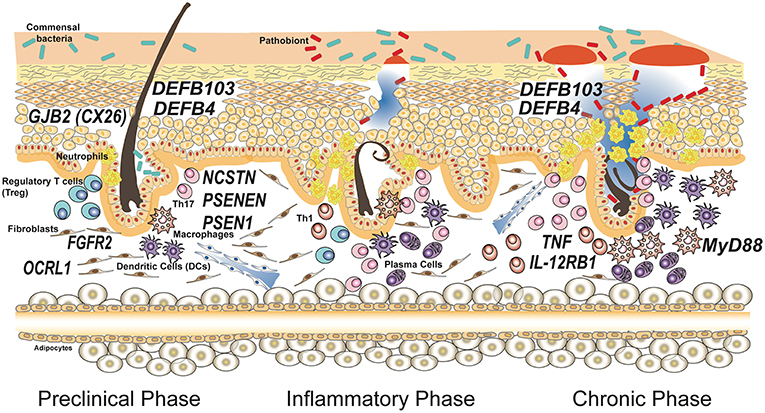
With HS, the hair follicle gets blocked through what is called follicular hyperkeratosis. This causes inflammation, which is partly due to bacteria on the skin but also due to activating the immune response due to damaged cells within the dermis.[ref]
A blocked hair follicle may bring to mind an ingrown hair from shaving, but instead of just a little inflammation, in HS, the body’s innate and adaptive immune system goes into overdrive. The inflammation causes an abscess to form, which destroys some of the adjacent cells, and the lesions persist.
Genetic component of hidradenitis suppurativa:
Genetics plays a big role in hidradenitis suppurativa with heritability estimated to be ~77% based on twin studies.[ref] Studies in fraternal twins show that genetic susceptibility is likely due to carrying multiple susceptibility variants rather than just a single mutation causing HS.[ref] This means that HS is caused by a combination of genetic susceptibility and environmental or lifestyle factors. Genetics alone doesn’t cause HS, and the same lifestyle factors alone won’t cause it for everyone.
Genes combine with environmental factors:
Lifestyle and environmental factors that increase the risk of HS include:[ref][ref]
- smoking
- being overweight or obese
- having insulin resistance or diabetes
- hormonal imbalance (which often goes along with obesity and insulin resistance)
Let’s dig into the details of what is going on with HS and the inflammatory pathways…
Inflammatory pathways activated in HS:
Research points to HS involving increased follicular keratosis which is thought to plug up hair cells. Then an inflammatory response causes the follicle cells to rupture, leading to more inflammation, pus, and pain.
The other theory of HS is that there is an auto-inflammatory condition that is driving the plugging of the hair follicle and subsequent pathology. The reasoning behind the theory that inflammation causes the plugged hair follicle is that subclinical inflammation often precedes HS.[ref]
Studies show that there are likely multiple pathways that end up causing HS. On the one hand, metabolic syndrome is strongly linked to HS, with bariatric surgery patients who are obese being at an almost 4-fold increase in relative risk of having HS. Inflammation is elevated in obesity and metabolic syndrome, and this drives the pathogenic response in HS.
The other side of the picture is that mutations in genes related to skin thickness as well as an inflammatory response are also at a high risk of HS.[ref]
Autoinflammatory diseases are rare genetic disorders that cause the immune system to overreact at times. One autoinflammatory disease connected to HS is familial Mediterranean fever, which is caused by mutations in the MEFV gene. A 2019 study found that individuals with a familial Mediterranean fever diagnosis were 45 times more likely to have HS.[ref][ref][ref]
Related article: Familial Mediterranean Fever
Inflammatory cytokines are elevated in biopsies of HS. Specifically, IL-17A, interferon-gamma, TNF-β, and TNF-alpha are inflammatory markers found in HS lesions.[ref][ref][ref] Genetic variants in the TNF gene that increase the inflammatory response have been shown to increase the risk of HS.
Related articles: TNF-alpha genetic variants and IL-17 genetic variants
The NLRP3 inflammasome is activated in skin samples from hidradenitis suppurativa patients. NLRP3 is a sensor that detects damaged cells or foreign particles and revs up the immune response. [ref][ref] Some people have a more active NLRP3 response due to genetic variants.
Related article: NLRP3 Inflammasome and chronic inflammation
Pyroptosis is the term for cell death from inflammation. The body has multiple ways of ‘killing’ damaged cells and recycling the contents. Pyroptosis is an inflammatory cell death that is initiated with the activation of the NLRP3 inflammasome. In addition to NLRP3 activation, a family of proteins called gasdermins are also involved. Gasdermins create pores in the cell membrane, causing the cell to rupture. Pyroptosis is the mechanism of cell death that drives more inflammation and the pathology of both hidradenitis suppurativa and psoriasis.[ref]
Genes related to the skin:
Several genetic variants related to skin cells have also been identified as increasing the risk of HS. These genetic changes increase keratin and the thickness of the outer layer of skin.
The GJB2 gene encodes a gap-junction protein that is important in both the skin and in the hair cells in the ear. Mutations in GJB2 can cause keratitis-ichthyosis-deafness (KID) syndrome, which causes hearing loss at an early age, thick nails, and skin lesions. Some individuals with KID syndrome also have a co-occurrence of hidradenitis suppurativa.[ref]
Variants in the SOX9 gene have also been identified as increasing susceptibility to HS. Overexpression of SOX9 causes increased skin thickening.[ref]
Co-morbid autoimmune conditions:
With a propensity for excessive inflammatory response, it is not surprising that individuals with HS are also more likely to have an autoimmune condition.
HS is more frequently found in people with: [ref]
- Inflammatory bowel disease (17% of Crohn’s patients have HS)
- Autoimmune joint diseases such as rheumatoid factor negative RA.
- Spondyloarthritis
- Lupus
- Mood disorders
Genotype report: Hidradenitis suppurativa susceptibility
Access this content:
An active subscription is required to access this content.
Lifehacks for HS:
Dietary changes, metabolic health, and weight loss:
Keto:
In a study involving 12 overweight women with HS, a low-carb ketogenic diet led to general improvements in body composition and in a reduction in the hidradenitis suppurativa scores within four weeks.[ref]
Carnivore:
Another study looked at the carnivore diet. This was an n=1 write-up of the results of an all-meat ketogenic diet. The patient reported that HS subsided within 43 days of strict adherence to a carnivore diet.[ref]
Weight loss generally helps with HS, but for some, the loose skin folds after weight loss can exacerbate the problem. Eliminating dairy has been shown to help some people with hidradenitis suppurative, and avoiding brewer’s yeast also helps some individuals.[ref]
Treatment options with clinical trials:
Biologics:
Often used for autoimmune disease, biologics suppress specific aspects of the immune system. Clinical trials are underway to evaluate these immunosuppressant medications for use in HS.[ref] Talk with your doctor about the options here, including the drawbacks of these types of drugs.
One study showed that people with TNF variants were more likely to respond to anti-TNF drugs.[ref]Check your TNF genetic variants below and see the full article on TNF for more details.
| Gene | RS ID | Your Genotype | Effect Allele | Effect Allele Frequency | Notes About Effect Allele |
|---|---|---|---|---|---|
| TNF | rs1800629 | -- | A | 0.15 | Increased TNF alpha, increased risk of many chronic inflammatory diseases |
| TNF | rs361525 | -- | A | 0.05 | Increased TNF alpha, increased risk of many chronic inflammatory diseases |
| TNF | rs1799964 | -- | C | 0.21 | Increased TNF alpha, increased risk of many chronic inflammatory diseases |
| TNF | rs1799724 | -- | T | 0.12 | Increased TNF alpha, increased risk of many chronic inflammatory diseases |
| TNFRSF1A | rs1800693 | -- | C | 0.39 | Increased risk of multiple sclerosis; increased NF-kB signaling |
| TNFRSF1A | rs767455 | -- | C | 0.42 | Increased risk of inflammatory diseases. |
| TNFRSF1B | rs1061622 | -- | G | 0.23 | Increased risk of psoriasis, lupus |
| TNF | rs1800610 | -- | A | 0.08 | Lower TNF; less inflammation but more susceptible to infectious diseases |
Antibiotic creams:
A clinical trial showed that clindamycin cream is effective for about 50% of HS patients.[ref]
Laser treatments:
Intense pulsed light with or without radio frequency reduces active lesion count after 3 months.[ref] Another study showed laser hair removal reduced HS scores in mild-to-moderate.[ref] A 2022 clinical trial showed that light therapy after antibiotic cream helped to maintain treatment success.[ref]
Methylene blue plus light therapy:
Access this content:
An active subscription is required to access this content.
Related articles and topics: