Key Takeaways:
~ The HLA-B27 serotype is linked to an increased risk of several autoimmune diseases, including ankylosing spondylitis, psoriatic arthritis, and IBD.
~Not everyone with HLA-B27 develops disease; environmental and other genetic factors also play a role.
~ You can check your 23 and Me or AncestryDNA raw data for the HLA-B27 genotype.
Why is HLA-B27 important?
HLA-B27 is a genetic marker that greatly increases the risk for ankylosing spondylitis and other autoimmune diseases. Carrying HLA-B27 increases your risk for certain autoimmune diseases, but it is not a diagnosis.
What is the HLA system?
Human leukocyte antigens (HLA) belong to the part of our immune system known as the major histocompatibility complex (MHC). The HLA genes code for the proteins that help our body determine the difference between a foreign invader that needs to be attacked and what is ‘self’.
People can have many different HLA serotypes, giving us all slightly different strengths and weaknesses against microbial diseases.
But along with attacking foreign invaders, a handful of HLA types also increase susceptibility to autoimmune diseases, where the body attacks its own cells.
HLA-B27: Why test for it?
Many people first hear about HLA-B27 from their doctor requesting a test for it. The test is a quick blood test to see whether you carry the HLA-B27 serotype. Usually, the doctor is looking to add strength to a probable diagnosis for certain autoimmune diseases.
How common is HLA B27 positive?
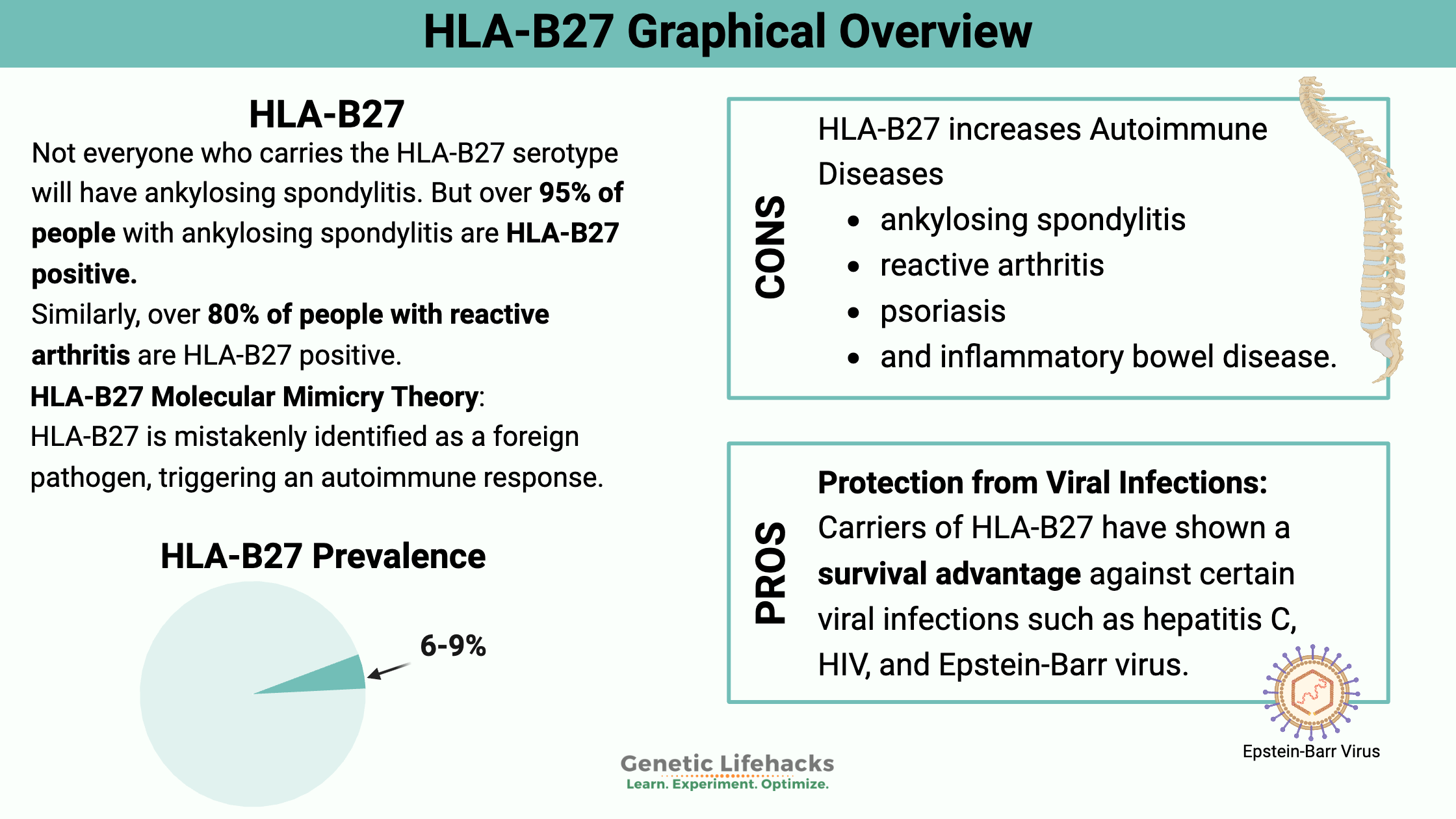
While the frequency of the HLA-B27 serotypes can vary a bit by ancestry, in general, about 6-9% of the population carries the HLA-B27 allele.[ref]
Positive HLA-B27 is not a diagnosis—other factors must be considered.
HLA-B27 and autoimmune diseases:
People who carry the HLA-B27 serotype are at an increased risk for inflammatory-related autoimmune diseases.
Autoimmune diseases associated with being HLA B27 positive include:
Post-infectious syndrome for shigellosis, salmonella, and chlamydia is also more common in people who are HLA-B27 positive. This is also known as reactive arthritis.[ref]
| Disease | Relative Risk if HLA-B27+ | % of Patients HLA-B27+ | Key Symptoms |
|---|---|---|---|
| Ankylosing spondylitis | 20-fold increase | >95% | Back pain, spinal stiffness |
| Reactive arthritis | Increased | >80% | Joint pain post-infection |
| Psoriatic arthritis | Increased | Variable | Skin and joint symptoms |
| IBD (Crohn’s, UC) | Increased | Variable | GI symptoms, joint pain |
| Uveitis | Increased | Variable | Eye inflammation |
Let’s dive into these in more detail.
What is ankylosing spondylitis (AS)?
Ankylosing spondylitis is a chronic inflammatory disease that mainly affects the spine. It causes back pain and spinal stiffness, and the vertebrae can fuse together. This often occurs in young adults. You can find more information on the Spondylitis Association of America site.
Carriers of HLA-B27 are at a 20-fold increased relative risk for ankylosing spondylitis.
Keep in mind that this is a relative risk. For example, if the risk of ankylosing spondylitis is normally 1 in 200 (0.5%), carrying the HLA-B27 variant increases your risk to 20 in 200 (10%). These are just example numbers… talk with your doctor about other risk factors.
Why is HLA-B27 linked to autoimmune diseases?
There are multiple subtypes of HLA-B27, and the specific types associated with ankylosing spondylitis include HLA-B*2701, HLA-B*2702, HLA-B*2704, HLA-B*2705, and HLA-B*2707.
Not everyone who carries the HLA-B27 serotype will have ankylosing spondylitis. But over 95% of people with ankylosing spondylitis are HLA-B27 positive.
Similarly, over 80% of people with reactive arthritis are HLA-B27 positive.[ref]
Therefore, the HLA-B27 serotype is a big risk factor for these autoimmune diseases, but it doesn’t cause the autoimmune disease by itself.
Instead, other factors must be involved that trigger the disease, such as toxicant exposure, pathogens, gut microbiome changes, diet, or lifestyle factors.[ref]
Proteins in the body, including the HLA proteins, are made up of amino acids that join and then fold up in a particular way. Researchers have found that HLA-B27 tends to misfold.
The specific subtypes of HLA-B27 associated with autoimmune diseases are likely to be misfolded or unfolded, causing problems when formed in the endoplasmic reticulum (ER).
The misfolded or unfolded proteins in the endoplasmic reticulum cause stress in that organelle. Researchers theorize that the body’s unfolded protein response mechanism causes inflammation.[ref]
HLA-B27 and the immune system:
Why is HLA-B27 linked to an increased risk of autoimmune diseases?
Misfolded proteins:
Researchers theorize that the HLA-B27 protein often misfolds, which triggers the cells to initiate what is called the unfolded protein response. Essentially, this is the process by which proteins that aren’t formed correctly are broken down, and the amino acids are recycled. When this unfolded protein response is activated too often, such as with HLA-B27, it triggers the inflammatory response with the IL-23/IL-17 pathway.[ref]
Inflammatory Pathways (IL23/IL17/TNF)
Recent research shows that the IL-23/IL-17 inflammatory pathway is likely involved in many spondyloarthritis-associated autoimmune diseases for which HLA-B27 increases the risk. TNF-alpha, another inflammatory cytokine, may also increase the risk of these spondyloarthritis-associated autoimmune diseases.[ref]
Related article: Genetic variants that increase TNF-alpha
IL-17 and Autoimmune diseases
Molecular mimicry?
At one point, researchers advanced a theory that HLA-B27 seemed similar to an infecting bacterial pathogen and thus caused autoimmune diseases. The idea is called ‘molecular mimicry’ and the reason the immune system attacks ‘self’ thinking it is a bacteria.
The problem is that newer research shows that you can create ankylosing spondylitis in an animal model without the T-cells needed to attack a pathogen. Thus, researchers are now uncertain whether molecular mimicry is the cause of ankylosing spondylitis.[ref][ref]
Positive side: Protection from viral infections
A lot of ‘bad’ mutations exist in the genome because they also create a benefit for survival. For example, a mutation that helps someone survive a pathogenic cholera outbreak means the person carrying the mutation lives to pass it on to their kids. Much of our genome is sculpted by surviving against bacterial or viral pathogens; if our ancestors hadn’t survived, we wouldn’t be here today.
Hepatitis C protection:
Interestingly, carriers of the HLA-B27 have a survival advantage and are likely to live longer with hepatitis C infections and with HIV.[ref][ref]
EBV protection:
Additionally, people with the HLA-B27 serotype may mount a better response against the Epstein-Barr virus.[ref]
Related article: Epstein-Barr Virus, Genetics and Reactivation
HLA-B27 Genotype Report
Genetic variants included in 23andMe and AncestryDNA data coding for HLA-B27 are listed below. These variants show if you are likely to carry an HLA-B27 type. A blood test is still needed to be 100% certain that you carry the exact HLA-B27 type associated with autoimmune diseases.
Access this content:
An active subscription is required to access this content.
Lifehacks: Probiotics and Perspective
Keep it in perspective:
Don’t freak out if you are a carrier of HLA-B27. Instead, use this information as a heads-up not to ignore health issues such as back pain.
Blood tests to confirm:
If you want to get the blood test for HLA-B27 and can’t get it through your doctor, you can order it on your own in the US. UltaLab Tests is one place that I use. There are other websites as well, so shop around for the best price.
Understanding the risk:
Although HLA-B27 increases the relative risk of ankylosing spondylitis by 20-fold, it is still a rare disease, with about 1 in 2000 people having it.[ref] If you have the HLA-B27 serotype, the lifetime absolute risk is about 6-10%.[ref]
There are other genetic variants thought to be involved in susceptibility to ankylosing spondylitis, as well as environmental factors that increase the risk.[ref]
Gut microbiome connection to HLA-B27: Consider testing
Access this content:
An active subscription is required to access this content.
Related Articles and Topics:
Psoriasis Genes: How Genetics Point to Individualized Solutions
Rheumatoid Arthritis: Genetics, Root Causes, and Treatment Research
References:
“Ankylosing Spondylitis (Spondyloarthritis; Ankylosis) |myVMC.” HealthEngine Blog, 17 Sept. 2004, https://healthinfo.healthengine.com.au/ankylosing-spondylitis.
Buxton, Jane A., et al. “Genetic Determinants of Cocaine-Associated Agranulocytosis.” BMC Research Notes, vol. 8, June 2015, p. 240. PubMed Central, https://doi.org/10.1186/s13104-015-1219-4.
—. “Genetic Determinants of Cocaine-Associated Agranulocytosis.” BMC Research Notes, vol. 8, June 2015, p. 240. PubMed Central, https://doi.org/10.1186/s13104-015-1219-4.
Chen, Bin, et al. “Role of HLA-B27 in the Pathogenesis of Ankylosing Spondylitis.” Molecular Medicine Reports, vol. 15, no. 4, Apr. 2017, pp. 1943–51. PubMed Central, https://doi.org/10.3892/mmr.2017.6248.
—. “Role of HLA-B27 in the Pathogenesis of Ankylosing Spondylitis.” Molecular Medicine Reports, vol. 15, no. 4, Apr. 2017, pp. 1943–51. PubMed Central, https://doi.org/10.3892/mmr.2017.6248.
Colmegna, Inés, et al. “HLA-B27-Associated Reactive Arthritis: Pathogenetic and Clinical Considerations.” Clinical Microbiology Reviews, vol. 17, no. 2, Apr. 2004, pp. 348–69. PubMed Central, https://doi.org/10.1128/CMR.17.2.348-369.2004.
Dieleman, L. A., et al. “Lactobacillus GG Prevents Recurrence of Colitis in HLA-B27 Transgenic Rats after Antibiotic Treatment.” Gut, vol. 52, no. 3, Mar. 2003, pp. 370–76.
Evans, David M., et al. “Interaction between ERAP1 and HLA-B27 in Ankylosing Spondylitis Implicates Peptide Handling in the Mechanism for HLA-B27 in Disease Susceptibility.” Nature Genetics, vol. 43, no. 8, July 2011, pp. 761–67. PubMed Central, https://doi.org/10.1038/ng.873.
“Facebook Title.” SAA, https://spondylitis.org/about-spondylitis/types-of-spondylitis/ankylosing-spondylitis/. Accessed 11 Nov. 2021.
Ge, Shichao, et al. “HLA-B27 Modulates Intracellular Growth of Salmonella Pathogenicity Island 2 Mutants and Production of Cytokines in Infected Monocytic U937 Cells.” PLoS ONE, vol. 7, no. 3, Mar. 2012, p. e34093. PubMed Central, https://doi.org/10.1371/journal.pone.0034093.
Haroon, Nigil. “Does a Positive HLA-B27 Test Increase Your Risk of Mortality?” The Journal of Rheumatology, vol. 42, no. 4, Apr. 2015, pp. 559–60. www.jrheum.org, https://doi.org/10.3899/jrheum.150017.
Joshi, Reeti, et al. “Is There a Higher Genetic Load of Susceptibility Loci in Familial Ankylosing Spondylitis?” Arthritis Care & Research, vol. 64, no. 5, May 2012, pp. 780–84. PubMed Central, https://doi.org/10.1002/acr.21601.
—. “Is There a Higher Genetic Load of Susceptibility Loci in Familial Ankylosing Spondylitis?” Arthritis Care & Research, vol. 64, no. 5, May 2012, pp. 780–84. PubMed Central, https://doi.org/10.1002/acr.21601.
Larson, Theresa, et al. “Emerging Drugs for Uveitis.” Expert Opinion on Emerging Drugs, vol. 16, no. 2, June 2011, pp. 309–22. PubMed Central, https://doi.org/10.1517/14728214.2011.537824.
Lin, Phoebe, et al. “HLA-B27 and Human Β2-Microglobulin Affect the Gut Microbiota of Transgenic Rats.” PLoS ONE, vol. 9, no. 8, Aug. 2014, p. e105684. PubMed Central, https://doi.org/10.1371/journal.pone.0105684.
—. “HLA-B27 and Human Β2-Microglobulin Affect the Gut Microbiota of Transgenic Rats.” PLoS ONE, vol. 9, no. 8, Aug. 2014, p. e105684. PubMed Central, https://doi.org/10.1371/journal.pone.0105684.
Lin, Zhiming, et al. “A Genome-Wide Association Study in Han Chinese Identifies New Susceptibility Loci for Ankylosing Spondylitis.” Nature Genetics, vol. 44, no. 1, Dec. 2011, pp. 73–77. PubMed, https://doi.org/10.1038/ng.1005.
—. “A Genome-Wide Association Study in Han Chinese Identifies New Susceptibility Loci for Ankylosing Spondylitis.” Nature Genetics, vol. 44, no. 1, Dec. 2011, pp. 73–77. PubMed, https://doi.org/10.1038/ng.1005.
Macfarlane, Tatiana V., et al. “Relationship between Diet and Ankylosing Spondylitis: A Systematic Review.” European Journal of Rheumatology, vol. 5, no. 1, Mar. 2018, pp. 45–52. PubMed Central, https://doi.org/10.5152/eurjrheum.2017.16103.
Mandour, Mohamed, et al. “The Role of the IL-23/IL-17 Axis in Disease Initiation in Spondyloarthritis: Lessons Learned From Animal Models.” Frontiers in Immunology, vol. 12, June 2021, p. 618581. PubMed Central, https://doi.org/10.3389/fimmu.2021.618581.
Roberts, Rebecca L., et al. “Prevalence of HLA-B27 in the New Zealand Population: Effect of Age and Ethnicity.” Arthritis Research & Therapy, vol. 15, no. 5, 2013, p. R158. PubMed Central, https://doi.org/10.1186/ar4341.
Sheehan, Nicholas J. “The Ramifications of HLA-B27.” Journal of the Royal Society of Medicine, vol. 97, no. 1, Jan. 2004, pp. 10–14.
Singh, Animesh, and Sarah Karrar. “The Role of Intracellular Organisms in the Pathogenesis of Inflammatory Arthritis.” International Journal of Inflammation, vol. 2014, 2014, p. 158793. PubMed Central, https://doi.org/10.1155/2014/158793.
Sorrentino, Rosa, et al. “HLA-B27 and Antigen Presentation: At the Crossroads between Immune Defense and Autoimmunity.” Molecular Immunology, vol. 57, no. 1, Jan. 2014, pp. 22–27. PubMed, https://doi.org/10.1016/j.molimm.2013.06.017.
Stoll, Matthew L., et al. “Age and Fecal Microbial Strain-Specific Differences in Patients with Spondyloarthritis.” Arthritis Research & Therapy, vol. 20, 2018, p. 14. PubMed Central, https://doi.org/10.1186/s13075-018-1510-6.
Vitulano, C., et al. “The Interplay between HLA‐B27 and ERAP1/ERAP2 Aminopeptidases: From Anti‐viral Protection to Spondyloarthritis.” Clinical and Experimental Immunology, vol. 190, no. 3, Dec. 2017, pp. 281–90. PubMed Central, https://doi.org/10.1111/cei.13020.
—. “The Interplay between HLA‐B27 and ERAP1/ERAP2 Aminopeptidases: From Anti‐viral Protection to Spondyloarthritis.” Clinical and Experimental Immunology, vol. 190, no. 3, Dec. 2017, pp. 281–90. PubMed Central, https://doi.org/10.1111/cei.13020.
Zhu, Wei, et al. “Ankylosing Spondylitis: Etiology, Pathogenesis, and Treatments.” Bone Research, vol. 7, Aug. 2019, p. 22. PubMed Central, https://doi.org/10.1038/s41413-019-0057-8.
—. “Ankylosing Spondylitis: Etiology, Pathogenesis, and Treatments.” Bone Research, vol. 7, Aug. 2019, p. 22. PubMed Central, https://doi.org/10.1038/s41413-019-0057-8.
Originally published 07/2018. Updated 1/2020.