Key takeaways:
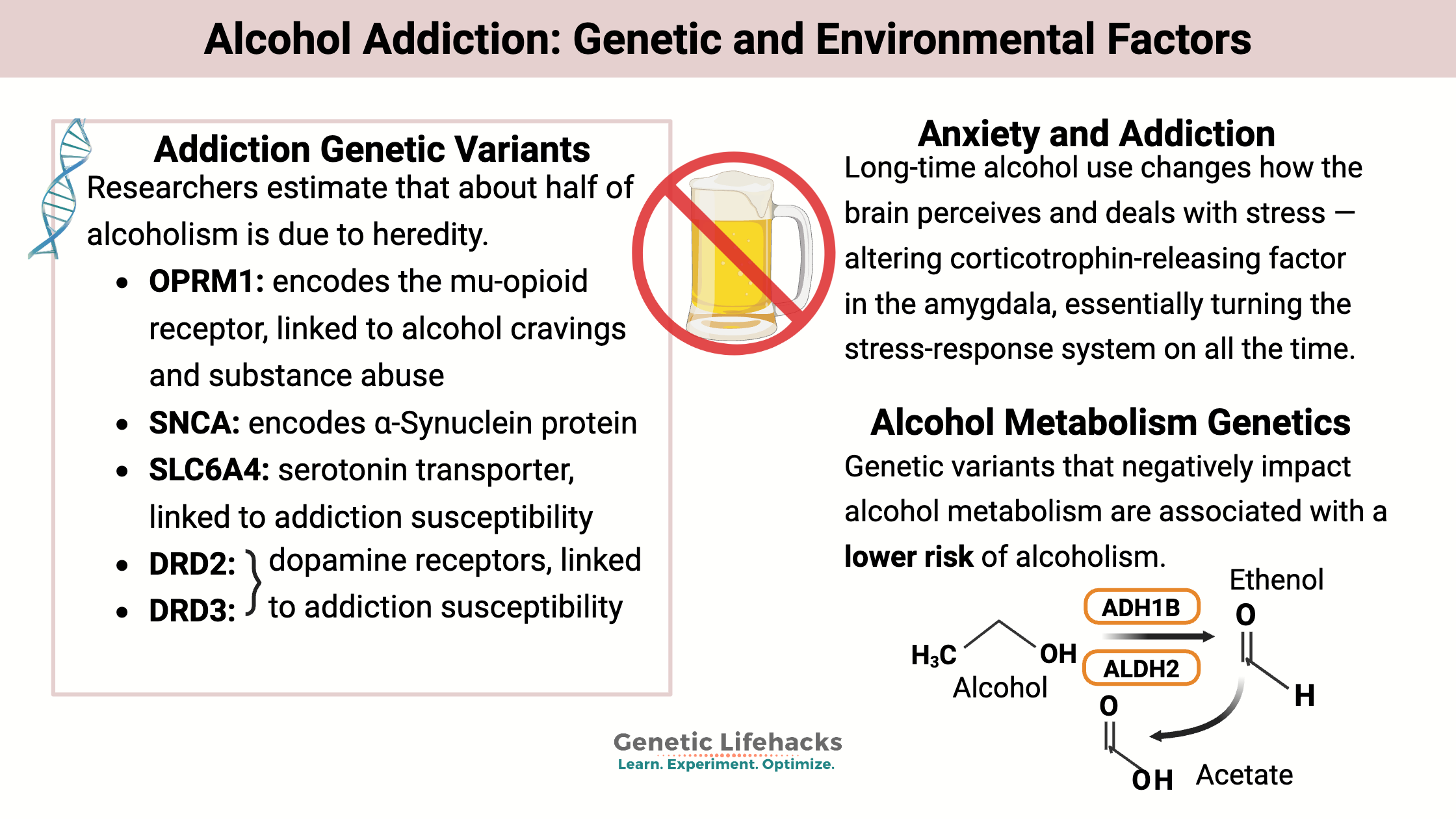
~ About half of the risk for alcohol use disorder (AUD) comes from genetic variants, while the other half is due to environmental influences such as stress, friends and family drinking habits, and negative life experiences.
~ While dopamine plays a role in the initial reward response to alcohol, long-term use alters the brain’s stress-response system. This can lead to a constant state of heightened stress, making withdrawal and relapse more likely.
~ Genetic variants in dopamine, serotonin, and alcohol metabolism genes influence susceptibility to alcoholism.
This article explores the genetic connections to alcohol addiction and includes research-backed treatment options. You’ll come away with an understanding of the physiological changes that are happening in the brain, and your genetic variants may point you toward the most effective treatment options.
Hereditary Component of Alcoholism
You may have heard it said that ‘alcoholism runs in the family’… And some families do have more alcohol abuse problems than others. For so many people, alcohol can wreak devastation on their lives — destroying their health, family relationships, longevity, and happiness.
Alcohol misuse is estimated to result in 3 million deaths worldwide each year (2016 numbers). Let that sink in…3 million people dying from overconsumption of alcohol. According to the World Health Organization: “Mortality resulting from alcohol consumption is higher than that caused by diseases such as tuberculosis, HIV/AIDS and diabetes.”[ref]
Is alcoholism a disease?
Alcoholism is now referred to as alcohol use disorder (AUD) or alcohol dependence. It is a diagnosable disease considered both physical and mental in nature.
While it is easy to dismiss alcohol dependence as being due to ‘not enough willpower’ or a ‘weakness’, the truth is, once established, alcohol dependence is due to physiological factors in addition to lifestyle.
One research study defines alcohol dependence as:
“Alcohol addiction is a chronic, relapsing brain disorder, which is characterized by a compulsion to seek alcohol, loss of control in limiting alcohol intake, and negative emotional state during withdrawal, in which genetic and environmental factors interact and appear to be equally important with respect to its development.”[ref]
Is alcoholism genetic or hereditary?
Sort of… the increased risk of alcohol use disorder is a combination of genetic variants and drinking history, lifestyle, and (often) abuse.
Researchers estimate that about half of alcoholism is due to heredity. The other half is due to environmental factors (stressful life events, access to alcohol, friends and family drinking, etc.).
Essentially, the genetic variants are related to addiction (dopamine and serotonin systems) and alcohol metabolism. In the Genetic Variants section below, I’ll explain the genes related to alcoholism in more detail.
Physical addiction to alcohol: Stress hormone system
Why is alcohol addictive? It turns out to be a more complex question to get solid answers about than I thought it would be.
Research on addiction has focused on dopamine and the ‘reward system’ in the brain for decades. In a nutshell, dopamine is released in a way to reinforce or reward the brain for a behavior. It makes you feel good, so you seek to do it again.
Research does seem to back up the idea that dopamine is involved in the initial addiction process for alcohol use disorder. It gives you a buzz, which is pleasant and rewarding (until the next morning). You feel less stressed, perhaps happier for a while. But dopamine isn’t the whole picture.
Alcohol eventually changes the brain’s wiring.
Corticotrophin-releasing factor is part of the hypothalamus-pituitary-adrenal (HPA) axis, controlling the release of stress hormones in response to anxiety-inducing situations. In people with long-time alcohol use, corticotrophin-releasing factor is altered in the amygdala. It changes how the brain perceives and deals with stress — essentially turning the stress-response system on all the time.[ref]
The link between anxiety and alcohol use is self-evident, and many people experience stress relief when drinking in a socially anxious situation. Research shows that people with anxiety disorders progress from normal alcohol consumption to alcohol use disorder faster than the average.[ref]
Related article: Is Anxiety Genetic?
Animal studies clearly show the changes in the brain due to upregulated corticotrophin-releasing factor. Researchers found that chronic alcohol exposure increases corticotropin-releasing factor receptors, and the effects are long-lasting, even after the withdrawal of alcohol. Moreover, long-term alcohol exposure also modifies brain plasticity and physically changes how the brain copes with stress.[ref]
Additionally, alcohol use disorder may result from other mental illnesses such as depression, bipolar disorder, or schizophrenia.[ref][ref]
Members: Check your mood disorder risk factors on the Mood and Brain Topic Summary Report
Alcohol Use Disorder Genotype Report:
Access this content:
An active subscription is required to access this content.
Lifehacks:
If you carry the genetic variants related to alcohol use disorder and don’t drink a lot, the obvious ‘lifehack’ here is to continue avoiding drinking alcohol. Know that genetic susceptibility is real and apply that logically. Plus, alcohol isn’t good for your liver, brain, or overall health.
Talking to your kids: If alcoholism runs in the family and you carry genetic variants that increase susceptibility, talk with your kids about it before they become teenagers. Please give them information about the heredity aspects of alcoholism to understand why they may be more at risk than their peers. Kids aren’t dumb, and giving them the facts about their risks is essential.
Getting the right help – Using genetics in alcohol use disorder.
If you have problems with drinking too much, please consider getting professional help.
- If you have a personal doctor, that’s the place to start. Prescription medications can help reduce drinking, and your doctor will also know the local resources available.
- In the US, there is a national treatment referral service hotline (confidential): 1-800-662-HELP (4357) or https://www.samhsa.gov/find-help/national-helpline. The Alcohol.org website also has a rehab admissions navigator that helps find a place that accepts your insurance.
- There are local alcohol abuse help services in every state and community-based organization in many places. You aren’t alone in this.
- Cognitive Behavior Therapy, along with medications, is beneficial for many, especially for people with anxiety disorders.[ref]
The Sinclair Method:
Naltrexone is an opioid receptor antagonist that is FDA-approved for alcohol dependence. Studies show that people with OPRM1 rs1799971 G-allele (in the genetics section above) respond better to naltrexone. G-allele carriers find that naltrexone blunts the cravings more.[ref]
Members: Your genotype for rs1799971 is —.
The Sinclair Method was developed in the 1990s by a researcher named Dr. Sinclair. It uses naltrexone before drinking to block the opioid receptor. This blunts the pleasant effects of alcohol, and eventually reduces the desire to drink. There are Sinclair Method coaches and support groups available to help people navigate their way through recovery from AUD.
Serotonin system (women):
Serotonin is also thought to be involved in alcohol addiction for some people. SSRIs seem to help reduce the number of drinks per day. When researchers looked at who really benefited from SSRIs, they found it worked best for women with a specific variable number tandem repeat in the serotonin receptor gene.[ref]
Variable number tandem repeats are not included in 23andMe or AncestryDNA data, but some SNPs usually go along with the serotonin transporter repeats (5HTTLPR). Thus you can get a pretty good idea of whether you have the long or short version of the serotonin receptor. A couple of studies have found that two SNPs predict the long or short version of 5-HTTLPR fairly well – around 95+% of the time.[ref][ref][ref]
| 5HTTLPR | rs2129785 (23andMe v4, v5; AncestryDNA) |
rs11867581 (23andMe v4, v5; AncestryDNA) |
|---|---|---|
| Long | T | G |
| Long | C | A |
| Short | T | A |
Your genotype for rs2129785 is —.
Your genotype for rs11867581 is —.
Examples:
- If your rs2129785 genotype is T/T and your rs11867581 genotype is A/G, you have one copy of the 5-HTTLPR short and one copy of the long version.
- If your rs2129785 genotype is T/T and your rs11867581 genotype is A/A, you have two copies of the 5-HTTLPR short.
- If your rs2129785 genotype is C/C and your rs11867581 genotype is A/G, you likely have two copies of the 5-HTTLPR long.
In a study on alcohol use disorder for women, the 5-HTTLPR length may help predict which medication works best:
- For women with 5HTTLPR Long/Long – ondansetron had better results
- For women with 5-HTTLPR Short/Short or Short/Long – sertraline (SSRI) had better results.[ref]
Supplements and Natural Options:
Let me be upfront here:
The research doesn’t show any prescription drug or natural supplement as a miracle cure for alcoholism for everyone. That said, supporting your overall health with nutrition and vitamins along with rehab or therapy may help make recovery easier.
Dihydromyricetin is a natural flavonoid supplement that counteracts alcohol withdrawal symptoms and reduces excessive alcohol consumption in animal studies.[ref] (I’m not finding any human clinical trials on it for alcohol, but it does help with fatty liver disease.)
Niacin:
A traditional supplement for alcoholism is niacin, which is vitamin B3. People who drink a lot tend to have nutrient deficiencies, including pellagra, which results from niacin deficiency.[ref]
Types of Niacin: When it comes to supplementing with niacin, several forms are available, including the older kind that makes you flush as well as non-flushing nicotinamide. Both seem to work for reversing niacin deficiency, so if you don’t like the flush, go with nicotinamide (also called niacinamide).
Liver protection:
Excess alcohol does bad things to the intestinal barrier (leaky gut) and the gut microbiome. It allows more bacteria to slip into the bloodstream, adding to liver problems in alcoholism. Additionally, alcohol increases gut motility (hangover diarrhea, the beer poops…).
Studies show that you can reduce liver problems in alcohol use disorder by supporting the intestinal barrier function with zinc, niacin, prebiotics, and probiotics. The prebiotics and probiotics help replenish the good bacteria that make short-chain fatty acids, which are needed to regenerate the intestinal cells. MCT oil may also help repair the gut and liver problems from alcohol.[ref]
Berberine:
Animal studies show that berberine may also help alter the gut microbiome in alcohol use disorder. Berberine is a natural plant compound used in regulating blood glucose levels, and it also helps with bacterial overgrowth.[ref]
B-vitamins:
A B-complex supplement may help to improve vitamin deficiencies. Alcoholism modifies several B-vitamin levels in the body (in addition to niacin). Both folate (B9) and B12 levels can be negatively impacted, and homocysteine may be elevated.[ref][ref]
Related article: Vitamin B12 genes
Thiamine deficiency is a big problem in alcoholism as well. Estimates range from 30-80% for thiamine deficiency in people with alcohol use disorder.[ref]
Related article: Thiamine genes
Whatever you choose to do, research shows that most interventions will help to reduce the number of drinks per day. Seek help, try multiple interventions, and take care of your overall health.[ref][ref]
Recap of your genes:
| Gene | RS ID | Your Genotype | Effect Allele | Effect Allele Frequency | Notes About Effect Allele |
|---|---|---|---|---|---|
| OPRM1 | rs1799971 | -- | G | 0.13 | Stronger alcohol cravings |
| SNCA | rs17015982 | -- | G | 0.09 | Increased risk of alcoholism |
| SLC6A4 | rs1042173 | -- | A | 0.54 | Stronger alcohol cravings |
| DRD2 | rs1076560 | -- | A | 0.14 | Increased risk of alcoholism |
| DRD3 | rs2134655 | -- | T | 0.24 | TT: Increased risk of alcoholism |
| GCKR | rs1260326 | -- | T | 0.4 | Slight Increased risk of alcoholism |
| KLB | rs11940694 | -- | A | 0.42 | Greater consumption |
| ADH1B | rs1229984 | -- | T | 0.04 | Reduced risk alcoholism |
| ADH1B | rs2066702 | -- | A | 0.01 | Reduced risk alcoholism |
| ALDH2 | rs671 | -- | A | 0.006 | Reduced risk alcoholism |
| ADH1C | rs698 | -- | C | 0.36 | Incr. risk pancreatitis |
Depression, bipolar disorder, and schizophrenia are also associated with a greater risk of alcoholism. Check your mood disorder risk factors:
Final thoughts:
If you are dealing with alcohol use disorder, please reach out to someone to help you. From Facebook groups on the Sinclair method to coaches who are trained to help to telemedicine therapists, there are so many more options available today. You don’t have to do it alone, and understanding the physiological reasons for AUD will hopefully help you realize that it is more than just ‘will power’.
Related Articles and Topics:
L-theanine for anxiety: genetics and nature’s chill pill
L-theanine is known for reducing anxiety and promoting sleep. Discover the many benefits of l-theanine and how supplementation might work for you.
Alcohol Genes: Alcohol Metabolism Rate
Wondering why you don’t react the same way to alcohol as your friends do? Some people metabolize alcohol faster, leaving a build-up of acetaldehyde. Learn more about why this can be a health problem for some. (Member’s article)
Metabolic Health Topic Summary Report
Metabolic health is important for your overall well-being. Learn how to optimize your health using your genes and our topic summary report.
Berberine: Research studies, Absorption, and Genetics
Berberine is a supplement that I’ve written about as a ‘Lifehack’ in a number of different articles. It is a natural compound with some amazing research on it in animal and cell studies, and it seems to be almost unbelievable. The drawback seems to be poor absorption in the intestines decreasing its effectiveness.
References:
Ait-Daoud, Nassima, et al. “Preliminary Evidence for Cue-Induced Alcohol Craving Modulated by Serotonin Transporter Gene Polymorphism Rs1042173.” Frontiers in Psychiatry, vol. 3, 2012, p. 6. PubMed, https://doi.org/10.3389/fpsyt.2012.00006.
Anton, Raymond F., et al. “An Evaluation of μ-Opioid Receptor (OPRM1) as a Predictor of Naltrexone Response in the Treatment of Alcohol Dependence: Results From the Combined Pharmacotherapies and Behavioral Interventions for Alcohol Dependence (COMBINE) Study.” Archives of General Psychiatry, vol. 65, no. 2, Feb. 2008, p. 135. www.ncbi.nlm.nih.gov, https://doi.org/10.1001/archpsyc.65.2.135.
Arias, Albert J., and R. Andrew Sewell. “Pharmacogenetically Driven Treatments for Alcoholism: Are We There Yet?” CNS Drugs, vol. 26, no. 6, June 2012, p. 461. www.ncbi.nlm.nih.gov, https://doi.org/10.2165/11633180-000000000-00000.
Arpawong, Thalida E., et al. “Effects of Recent Stress and Variation in the Serotonin Transporter Polymorphism (5-HTTLPR) on Depressive Symptoms: A Repeated-Measures Study of Adults Age 50 and Older.” Behavior Genetics, vol. 46, no. 1, Jan. 2016, pp. 72–88. PubMed Central, https://doi.org/10.1007/s10519-015-9740-8.
Badawy, Abdulla A. B. “Pellagra and Alcoholism: A Biochemical Perspective.” Alcohol and Alcoholism (Oxford, Oxfordshire), vol. 49, no. 3, June 2014, pp. 238–50. PubMed, https://doi.org/10.1093/alcalc/agu010.
Baumgartner, Christian, et al. “‘Take Care of You’ – Efficacy of Integrated, Minimal-Guidance, Internet-Based Self-Help for Reducing Co-Occurring Alcohol Misuse and Depression Symptoms in Adults: Results of a Three-Arm Randomized Controlled Trial.” Drug and Alcohol Dependence, vol. 225, Aug. 2021, p. 108806. PubMed, https://doi.org/10.1016/j.drugalcdep.2021.108806.
Blasco, Carmen, et al. “Prevalence and Mechanisms of Hyperhomocysteinemia in Chronic Alcoholics.” Alcoholism, Clinical and Experimental Research, vol. 29, no. 6, June 2005, pp. 1044–48. PubMed, https://doi.org/10.1097/01.alc.0000169265.36440.ee.
Edenberg, Howard J. “The Genetics of Alcohol Metabolism: Role of Alcohol Dehydrogenase and Aldehyde Dehydrogenase Variants.” Alcohol Research & Health, vol. 30, no. 1, 2007, pp. 5–13.
—. “The Genetics of Alcohol Metabolism: Role of Alcohol Dehydrogenase and Aldehyde Dehydrogenase Variants.” Alcohol Research & Health, vol. 30, no. 1, 2007, pp. 5–13.
—. “The Genetics of Alcohol Metabolism: Role of Alcohol Dehydrogenase and Aldehyde Dehydrogenase Variants.” Alcohol Research & Health, vol. 30, no. 1, 2007, pp. 5–13.
—. “The Genetics of Alcohol Metabolism: Role of Alcohol Dehydrogenase and Aldehyde Dehydrogenase Variants.” Alcohol Research & Health, vol. 30, no. 1, 2007, pp. 5–13.
Ehlers, Cindy L. “Variations in ADH and ALDH in Southwest California Indians.” Alcohol Research & Health, vol. 30, no. 1, 2007, pp. 14–17.
Fang, F., et al. “Association between Alcohol Dehydrogenase 1C Gene *1/*2 Polymorphism and Pancreatitis Risk: A Meta-Analysis.” Genetics and Molecular Research: GMR, vol. 14, no. 4, Nov. 2015, pp. 15267–75. PubMed, https://doi.org/10.4238/2015.November.30.2.
Heilig, Markus, et al. “Translating the Neuroscience of Alcoholism into Clinical Treatments: From Blocking the Buzz to Curing the Blues.” Neuroscience and Biobehavioral Reviews, vol. 35, no. 2, Nov. 2010, p. 334. www.ncbi.nlm.nih.gov, https://doi.org/10.1016/j.neubiorev.2009.11.018.
Janeczek, Paulina, et al. “Reduced Expression of α-Synuclein in Alcoholic Brain: Influence of SNCA-Rep1 Genotype.” Addiction Biology, vol. 19, no. 3, May 2014, p. 509. www.ncbi.nlm.nih.gov, https://doi.org/10.1111/j.1369-1600.2012.00495.x.
Kaner, Eileen Fs, et al. “Personalised Digital Interventions for Reducing Hazardous and Harmful Alcohol Consumption in Community-Dwelling Populations.” The Cochrane Database of Systematic Reviews, vol. 9, Sept. 2017, p. CD011479. PubMed, https://doi.org/10.1002/14651858.CD011479.pub2.
Kenna, George A., et al. “Ondansetron Reduces Naturalistic Drinking in Non-Treatment Seeking Alcohol Dependent Individuals with the LL 5′-HTTLPR Genotype: A Laboratory Study.” Alcoholism, Clinical and Experimental Research, vol. 38, no. 6, June 2014, p. 1567. www.ncbi.nlm.nih.gov, https://doi.org/10.1111/acer.12410.
—. “Ondansetron Reduces Naturalistic Drinking in Non-Treatment Seeking Alcohol Dependent Individuals with the LL 5′-HTTLPR Genotype: A Laboratory Study.” Alcoholism, Clinical and Experimental Research, vol. 38, no. 6, June 2014, p. 1567. www.ncbi.nlm.nih.gov, https://doi.org/10.1111/acer.12410.
Kranzler, Henry R., et al. “Genome-Wide Association Study of Alcohol Consumption and Use Disorder in 274,424 Individuals from Multiple Populations.” Nature Communications, vol. 10, no. 1, Apr. 2019, p. 1499. www.nature.com, https://doi.org/10.1038/s41467-019-09480-8.
Kushner, Matt G., Eric W. Maurer, et al. “Hybrid Cognitive Behavioral Therapy Versus Relaxation Training for Co-Occurring Anxiety and Alcohol Disorder: A Randomized Clinical Trial.” Journal of Consulting and Clinical Psychology, vol. 81, no. 3, June 2013, p. 429. www.ncbi.nlm.nih.gov, https://doi.org/10.1037/a0031301.
Kushner, Matt G., Eric Maurer, et al. “Vulnerability to the Rapid (‘Telescoped’) Development of Alcohol Dependence in Individuals with Anxiety Disorder.” Journal of Studies on Alcohol and Drugs, vol. 72, no. 6, Nov. 2011, p. 1019. www.ncbi.nlm.nih.gov, https://doi.org/10.15288/jsad.2011.72.1019.
Li, Dawei, et al. “Further Clarification of The Contribution of The ADH1C Gene to The Vulnerability of Alcoholism And Selected Liver Diseases.” Human Genetics, vol. 131, no. 8, Aug. 2012, pp. 1361–74. PubMed Central, https://doi.org/10.1007/s00439-012-1163-5.
—. “Strong Association of the Alcohol Dehydrogenase 1B Gene (ADH1B) with Alcohol Dependence and Alcohol-Induced Medical Diseases.” Biological Psychiatry, vol. 70, no. 6, Sept. 2011, pp. 504–12. PubMed, https://doi.org/10.1016/j.biopsych.2011.02.024.
Li, Sha, et al. “Modulation of Gut Microbiota Mediates Berberine‐induced Expansion of Immuno‐suppressive Cells to against Alcoholic Liver Disease.” Clinical and Translational Medicine, vol. 10, no. 4, Aug. 2020. www.ncbi.nlm.nih.gov, https://doi.org/10.1002/ctm2.112.
McHugh, R. Kathryn, and Roger D. Weiss. “Alcohol Use Disorder and Depressive Disorders.” Alcohol Research: Current Reviews, vol. 40, no. 1, Oct. 2019, p. arcr.v40.1.01. PubMed, https://doi.org/10.35946/arcr.v40.1.01.
SAMHSA’s National Helpline – 1-800-662-HELP (4357) | SAMHSA – Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/find-help/national-helpline. Accessed 18 Oct. 2021.
Sasabe, Toshikazu, et al. “Association Analysis of the Dopamine Receptor D2 (DRD2) SNP Rs1076560 in Alcoholic Patients.” Neuroscience Letters, vol. 412, no. 2, Jan. 2007, pp. 139–42. PubMed, https://doi.org/10.1016/j.neulet.2006.10.064.
Schumann, Gunter, et al. “KLB Is Associated with Alcohol Drinking, and Its Gene Product β-Klotho Is Necessary for FGF21 Regulation of Alcohol Preference.” Proceedings of the National Academy of Sciences, vol. 113, no. 50, Dec. 2016, pp. 14372–77. www.pnas.org, https://doi.org/10.1073/pnas.1611243113.
Sher, Leo, et al. “Clinical Features and Psychiatric Comorbidities in Military Veterans with Schizophrenia with or without Suicidality.” Journal of Psychiatric Research, vol. 143, Sept. 2021, pp. 262–67. PubMed, https://doi.org/10.1016/j.jpsychires.2021.09.028.
Siomek-Gorecka, Agnieszka, et al. “The Molecular Basis of Alcohol Use Disorder (AUD). Genetics, Epigenetics, and Nutrition in AUD: An Amazing Triangle.” International Journal of Molecular Sciences, vol. 22, no. 8, Apr. 2021. www.ncbi.nlm.nih.gov, https://doi.org/10.3390/ijms22084262.
—. “The Molecular Basis of Alcohol Use Disorder (AUD). Genetics, Epigenetics, and Nutrition in AUD: An Amazing Triangle.” International Journal of Molecular Sciences, vol. 22, no. 8, Apr. 2021. www.ncbi.nlm.nih.gov, https://doi.org/10.3390/ijms22084262.
van den Wildenberg, Esther, et al. “A Functional Polymorphism of the Mu-Opioid Receptor Gene (OPRM1) Influences Cue-Induced Craving for Alcohol in Male Heavy Drinkers.” Alcoholism, Clinical and Experimental Research, vol. 31, no. 1, Jan. 2007, pp. 1–10. PubMed, https://doi.org/10.1111/j.1530-0277.2006.00258.x.
Vinkhuyzen, Anna A. E., et al. “Identification of Tag Haplotypes for 5HTTLPR for Different Genome-Wide SNP Platforms.” Molecular Psychiatry, vol. 16, no. 11, Nov. 2011, pp. 1073–75. PubMed Central, https://doi.org/10.1038/mp.2011.68.
—. “Identification of Tag Haplotypes for 5HTTLPR for Different Genome-Wide SNP Platforms.” Molecular Psychiatry, vol. 16, no. 11, Nov. 2011, pp. 1073–75. PubMed Central, https://doi.org/10.1038/mp.2011.68.
Xu, Hong, et al. “Effects of Chronic Voluntary Alcohol Drinking on Thiamine Concentrations, Endoplasmic Reticulum Stress and Oxidative Stress in the Brain of Crossed High Alcohol Preferring Mice.” Neurotoxicity Research, vol. 36, no. 4, Nov. 2019, p. 777. www.ncbi.nlm.nih.gov, https://doi.org/10.1007/s12640-019-00032-y.
Yang, Hsin-Chou, et al. “Using an Event-History with Risk-Free Model to Study the Genetics of Alcoholism.” Scientific Reports, vol. 7, 2017. www.ncbi.nlm.nih.gov, https://doi.org/10.1038/s41598-017-01791-4.
Zhou, Zhanxiang, and Wei Zhong. “Targeting the Gut Barrier for the Treatment of Alcoholic Liver Disease.” Liver Research, vol. 1, no. 4, Dec. 2017, p. 197. www.ncbi.nlm.nih.gov, https://doi.org/10.1016/j.livres.2017.12.004.
Debbie Moon is a biologist, engineer, author, and the founder of Genetic Lifehacks where she has helped thousands of members understand how to apply genetics to their diet, lifestyle, and health decisions. With more than 10 years of experience translating complex genetic research into practical health strategies, Debbie holds a BS in engineering from Colorado School of Mines and an MSc in biological sciences from Clemson University. She combines an engineering mindset with a biological systems approach to explain how genetic differences impact your optimal health.