Key takeaways:
~ Recent headlines have touted that meat consumption causes colon cancer.
~ Research studies, though, show that only part of the population is at an increased risk of colon cancer from processed meat due to specific genetic variants.
~ Understanding your genes can help you know how processed meat will affect your risk of colon cancer.
Colon cancer, red meat, and personalized nutrition:
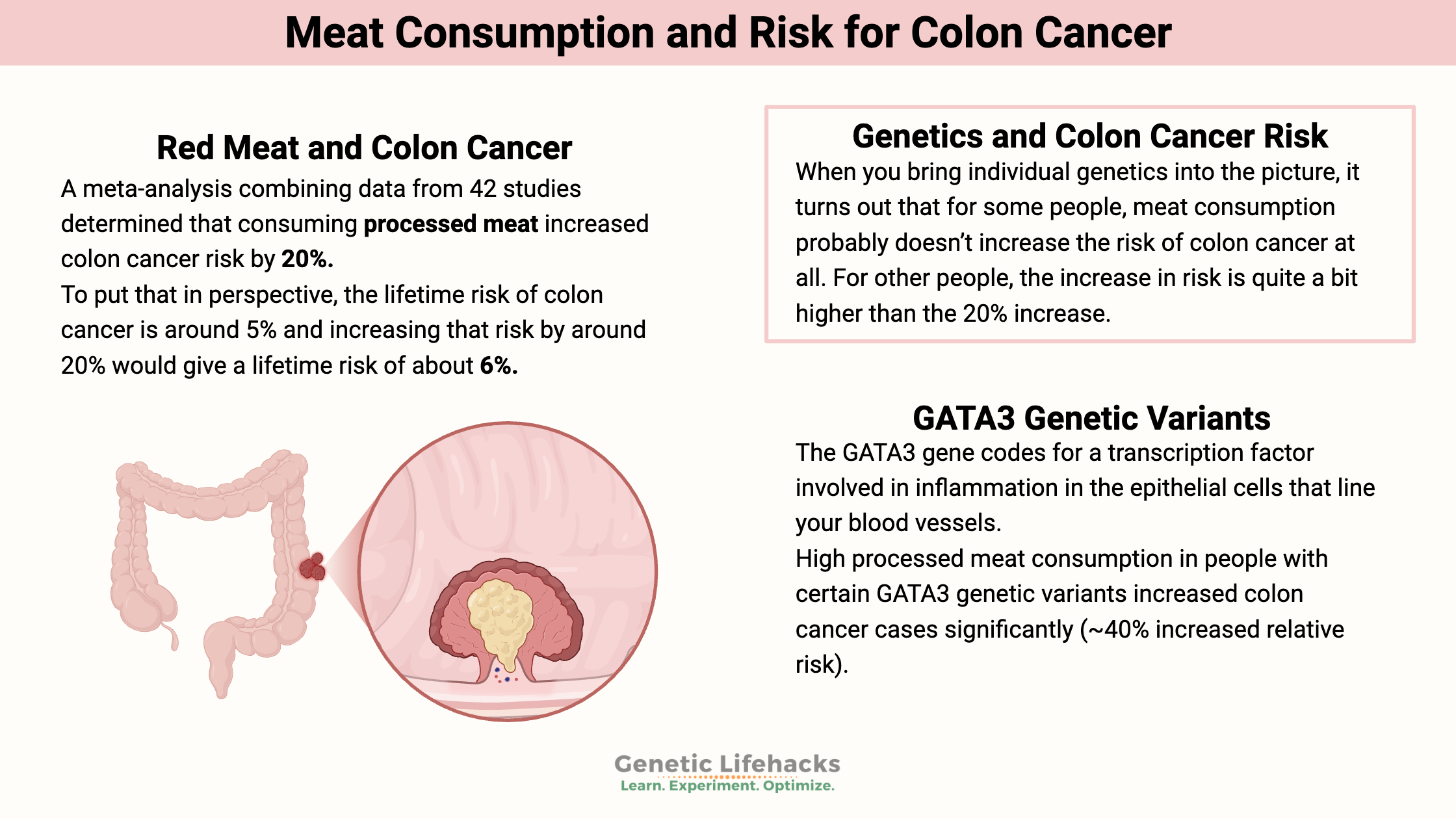
In 2015, the World Health Organization added processed meat (e.g., sausages, ham, hot dogs, beef jerky) to its list of probable carcinogens.[ref] The listing is based on several large epidemiological studies that show processed meat consumption increases the relative risk of colon cancer by 18-20%.
For example, a meta-analysis combining data from 42 studies determined that consuming processed meat increased colon cancer risk by 20%.[ref]
Putting the risk into perspective:
According to the American Cancer Society, the lifetime risk of colon cancer is around 5%, and increasing that risk by around 20% would give a lifetime risk of about 6%.[ref]
Importantly, this statistical risk is based on epidemiological studies of the population as a whole. It doesn’t take into account individual genetic variants that can increase – or decrease – the risk of colon cancer.
When you bring individual genetics into the picture, it turns out that for some people, meat consumption probably doesn’t increase the risk of colon cancer at all. However, people with specific genetic variants may have a much higher increase in colon cancer risk.
Genetics and colon cancer risk:
A 2014 study looked at the interaction between genetics and the risk of colon cancer from processed meat intake. Researchers examined the genes of 9,000 colon cancer patients and 9,000 control subjects without colon cancer. They discovered a significant diet-gene interaction between the GATA3 gene variants and colon cancer risk when stratified by meat consumption (processed meat and red meat).[ref]
Another study found that a genetic variant in the CCAT gene normally decreased the risk of colon cancer, but in conjunction with a high intake of processed meat, that protection was eliminated. [ref]
Polyps and meat intake:
Colorectal polyps are often precursors for colon cancer. These are the growths that doctors remove when you get a colonoscopy done in order to prevent cancer. Not all polyps go on to become cancerous, but polypectomy is a well-studied prevention method.
Red meat intake is associated with polyps, and genetic variants impact whether red meat is likely to cause you to have polyps. The aryl hydrocarbon receptor (AhR) is an important detector of toxicants, such as polycyclic aromatic hydrocarbons from high-temperature meat cooking. Polycyclic aromatic hydrocarbons are linked to the DNA changes that can cause benign polyps and malignant tumors.[ref]
Colon Cancer and Meat Genotype Report:
Access this content:
An active subscription is required to access this content.
Lifehacks:
If you carry the risk alleles above – especially if you have a family history of colon cancer – consider cutting down on or eliminating processed meats from your diet.
Examples of processed meat include:
- brats
- lunch meat
- bacon
- pepperoni
- salami
- hotdogs
Access this content:
An active subscription is required to access this content.
Related Articles and Topics:
GSTs: glutathione-S-transferase enzymes for detoxifying environmental toxins
Your body has fascinating ways of breaking down and eliminating toxicants, medications, and even hormones made in the body. The glutathione S-transferase genes code for enzymes involved in the removal of a variety of carcinogens and environmental toxins.
Aspirin, colon cancer, and genetics
Colon cancer is one of the most common forms of cancer, with a lifetime risk of about 5%. The good news is that survival rates are high for those who detect it early. Aspirin is dirt cheap and has been used for hundred-plus years. Recently, it has been in the news as possibly preventing several types of cancer, including colon cancer.
Originally published 1/2018; updated 8/2020