Key takeaways:
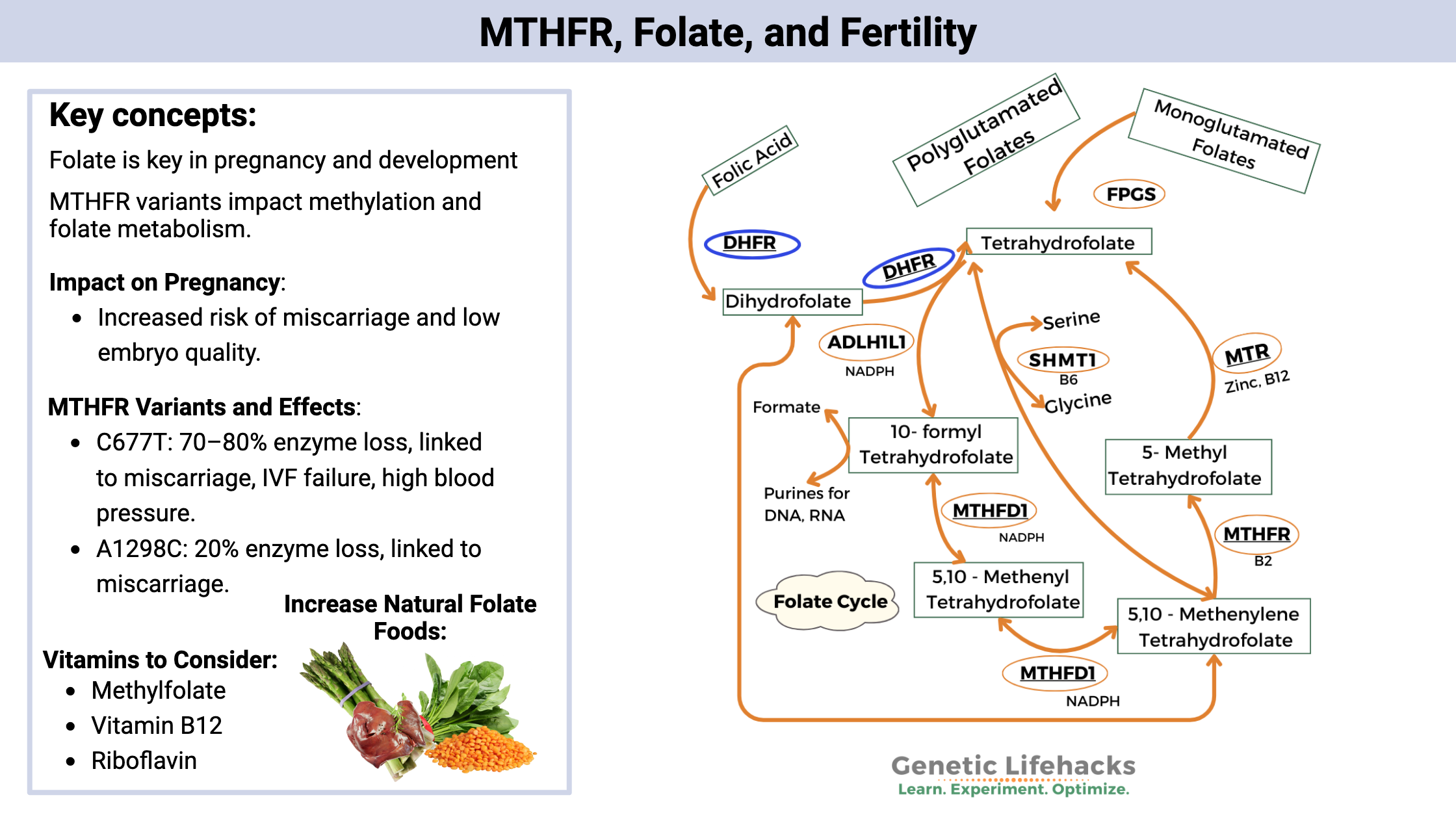
~ MTHFR variants are common and cause a decrease in the enzyme that converts folate into the active form, methylfolate.
~ Methylfolate is essential in many different cellular reactions.
~ Optimizing folate intake is an easy way to improve health and improve egg quality.
Getting pregnant with MTHFR
MTHFR is a gene that encodes methylenetetrahydrofolate reductase, an enzyme that converts folate to 5-methyltetrahydrofolate (or methylfolate) for use in the methylation cycle. The issue is that a percentage of the population has a variant of MTHFR that reduces its ability to function optimally, thereby affecting the methylation cycle.
What’s the big deal about the methylation cycle?
A methyl group is made up of three hydrogen atoms linked together by a carbon atom (CH3). Simple, but essential to many processes in our bodies.
The methylation cycle is how our body makes methyl groups. Methyl groups are required for various biochemical processes such as detoxification, neurotransmitter conversion, DNA synthesis, gene silencing, and histamine and estrogen metabolism. Methylation reactions involve transferring a methyl group to the molecule that requires it.
SAMe (s-adenosylmethionine) is the major methyl donor in cells. It donates a methyl group to other substances that need it.
The methylation cycle, though, hinges on SAMe getting enough methyl groups.
Folate can be used as a methyl donor. It is converted into methylfolate using the MTHFR enzyme.
If you carry an MTHFR variant that causes a decreased ability to create methylfolate, this can become the sticking point in the methylation cycle.[ref]
How does MTHFR relate to infertility?
Pregnancy is a time of increased need for folate. Methyl groups are needed for nucleotide synthesis in the developing baby.[ref]
Research shows that women who carry the MTHFR variants are at an increased risk for miscarriage. A meta-analysis of over 57 different studies found that both MTHFR C677T and A1298C were associated with an increased risk of miscarriage.[ref]
The MTHFR C677T variant also influences IVF success rates. Women with two copies of the C677T variant (rs1801133, AA genotype) are at a more than double risk for recurrent implantation failure in IVF and have fewer transferable embryos.[ref][ref]
Women with MTHFR C677T variants are also at an increased risk of high blood pressure during pregnancy.[ref]
A recent study identified another MTHFR variant associated with low ovarian reserve.[ref] Low ovarian reserve is also called low egg count and occurs when the ovaries lose their reproductive potential.
Why are pregnant women encouraged to take folate?
Several decades ago, researchers made the connection between low folate status and an increased risk of neural tube defects or cleft lips in babies. During the development process, a lot of nutrients and energy are required, including folate and methyl groups. Folic acid was added to wheat and rice products in the 1990s in an effort to decrease neural tube defects.
Related article: Folic acid vs. methylfolate
MTHFR C677T Genotype Report:
Lifehacks: Natural Solutions for MTHFR when trying to get pregnant
While the MTHFR variant is associated with an increased risk of miscarriage, this risk can be eliminated by consuming enough folate to meet your body’s requirements. This is one genetic variant that can be mitigated through diet and supplements.
While folate is essential for all women trying to conceive, it is especially critical for women with MTHFR mutations. Leafy green vegetables and legumes are excellent sources of folate. Beef liver also packs a ton of folate in it.
Related article: Recipes and folate-rich foods for MTHFR
Note that I keep saying ‘folate’ rather than folic acid. Folic acid is a synthetic form of folate that is used in many vitamins and to fortify wheat products in the United States.
Folic acid in excess could be detrimental in women with the MTHFR C677T mutation. In fact, some studies indicate that unmetabolized folic acid can accumulate and be harmful.[ref] Check the ingredients on any prenatal supplements, and talk with your fertility specialist if you have questions.
Methylfolate is the active form that bypasses the need for the MTHFR enzyme.
A study of women undergoing infertility treatment found that a B-complex with methylfolate improved pregnancy and birth rates compared to women taking folic acid supplements.[ref]
Related Articles and Topics:
Lithium Orotate and Mood:
Find out how low-dose lithium orotate interacts with vitamin B12 and can impact mood for some people.
Estrogen, histamine, and mast cells:
Mast cells have estrogen receptors and may be more easily triggered when estrogen (or estrogen-mimicking compounds) are high.
Lipoprotein a: How to check your genetic data
High Lp(a) levels are a big risk factor for sudden heart attacks. Your Lp(a) levels are mainly controlled by your genetic variants. Check to see if you carry genetic variants that increase or decrease Lp(a).
References:
Aneji, Chiamaka N., et al. “Deep Sequencing Study of the MTHFR Gene to Identify Variants Associated with Myelomeningocele.” Birth Defects Research. Part A, Clinical and Molecular Teratology, vol. 94, no. 2, Feb. 2012, pp. 84–90. PubMed, https://doi.org/10.1002/bdra.22884.
Bueno, Olalla, et al. “Common Polymorphisms That Affect Folate Transport or Metabolism Modify the Effect of the MTHFR 677C > T Polymorphism on Folate Status.” The Journal of Nutrition, vol. 146, no. 1, Jan. 2016, pp. 1–8. PubMed, https://doi.org/10.3945/jn.115.223685.
Choi, Youngsok, et al. “Genetic Variation of Methylenetetrahydrofolate Reductase (MTHFR) and Thymidylate Synthase (TS) Genes Is Associated with Idiopathic Recurrent Implantation Failure.” PLoS ONE, vol. 11, no. 8, Aug. 2016, p. e0160884. PubMed Central, https://doi.org/10.1371/journal.pone.0160884.
Christensen, Karen E., et al. “High Folic Acid Consumption Leads to Pseudo-MTHFR Deficiency, Altered Lipid Metabolism, and Liver Injury in Mice.” The American Journal of Clinical Nutrition, vol. 101, no. 3, Mar. 2015, pp. 646–58. PubMed, https://doi.org/10.3945/ajcn.114.086603.
Cirillo, Michela, et al. “5-Methyltetrahydrofolate and Vitamin B12 Supplementation Is Associated with Clinical Pregnancy and Live Birth in Women Undergoing Assisted Reproductive Technology.” International Journal of Environmental Research and Public Health, vol. 18, no. 23, Nov. 2021, p. 12280. PubMed Central, https://doi.org/10.3390/ijerph182312280.
de Aquino, Sibele Nascimento, et al. “MTHFR Rs2274976 Polymorphism Is a Risk Marker for Nonsyndromic Cleft Lip with or without Cleft Palate in the Brazilian Population.” Birth Defects Research. Part A, Clinical and Molecular Teratology, vol. 100, no. 1, Jan. 2014, pp. 30–35. PubMed, https://doi.org/10.1002/bdra.23199.
Gong, Mancheng, et al. “MTHFR 677C>T Polymorphism Increases the Male Infertility Risk: A Meta-Analysis Involving 26 Studies.” PLoS ONE, vol. 10, no. 3, Mar. 2015, p. e0121147. PubMed Central, https://doi.org/10.1371/journal.pone.0121147.
Jankovic-Karasoulos, Tanja, et al. “Maternal Folate, One-Carbon Metabolism and Pregnancy Outcomes.” Maternal & Child Nutrition, vol. 17, no. 1, Jan. 2021, p. e13064. PubMed, https://doi.org/10.1111/mcn.13064.
Pietrzik, K. F., and B. Thorand. “Folate Economy in Pregnancy.” Nutrition (Burbank, Los Angeles County, Calif.), vol. 13, no. 11–12, 1997, pp. 975–77. PubMed, https://doi.org/10.1016/s0899-9007(97)00340-7.
Raghavan, Ramkripa, et al. “Maternal Multivitamin Intake, Plasma Folate and Vitamin B 12 Levels and Autism Spectrum Disorder Risk in Offspring.” Paediatric and Perinatal Epidemiology, vol. 32, no. 1, Jan. 2018, pp. 100–11. DOI.org (Crossref), https://doi.org/10.1111/ppe.12414.
Vagnini, Laura D., et al. “Correlation of TP53 (Rs1625895), TP73 (Rs3765730), MMP9 (Rs17576), and MTHFR (Rs868014) Polymorphisms with Low Ovarian Reserve.” European Journal of Obstetrics, Gynecology, and Reproductive Biology, vol. 269, Feb. 2022, pp. 132–37. PubMed, https://doi.org/10.1016/j.ejogrb.2021.08.034.
Yang, Yi, et al. “Association between Maternal, Fetal and Paternal MTHFR Gene C677T and A1298C Polymorphisms and Risk of Recurrent Pregnancy Loss: A Comprehensive Evaluation.” Archives of Gynecology and Obstetrics, vol. 293, no. 6, June 2016, pp. 1197–211. PubMed, https://doi.org/10.1007/s00404-015-3944-2.
Zeng, Hong, et al. “MTHFR 677TT Is Associated with Decreased Number of Embryos and Cumulative Live Birth Rate in Patients Undergoing GnRHa Short Protocol: A Retrospective Study.” BMC Pregnancy and Childbirth, vol. 22, Mar. 2022, p. 170. PubMed Central, https://doi.org/10.1186/s12884-022-04506-4.
Zhang, Donghong, et al. “Elevated Homocysteine Level and Folate Deficiency Associated with Increased Overall Risk of Carcinogenesis: Meta-Analysis of 83 Case-Control Studies Involving 35,758 Individuals.” PloS One, vol. 10, no. 5, 2015, p. e0123423. PubMed, https://doi.org/10.1371/journal.pone.0123423.
Zhang, Ling, et al. “Status of Maternal Serum B Vitamins and Pregnancy Outcomes: New Insights from in Vitro Fertilization and Embryo Transfer (IVF-ET) Treatment.” Frontiers in Nutrition, vol. 9, 2022, p. 962212. PubMed, https://doi.org/10.3389/fnut.2022.962212.