One recommendation often made for lowering cholesterol levels is to consume higher amounts of plant sterols. You can find plant sterols in supplements such as beta-sitosterol or spreads like Benecol or SmartBalance margarine. These butter alternatives are marketed as a heart-healthy way to help you lower cholesterol and prevent cardiovascular disease (CVD).
It turns out that plant sterols probably lower cholesterol only in people with certain genetic variants. Plus, in an interesting twist, people with genetic variants that cause greatly increased plant sterol levels are actually at a higher risk of atherosclerosis and CVD.
So the question is – are plant sterols good or bad for you? The answer depends, in part, on your genes. Let’s dig into the science here so that you can make better choices than just relying on product marketing for your health decisions. Members will see their genotype report below, plus additional solutions in the Lifehacks section. Join today.
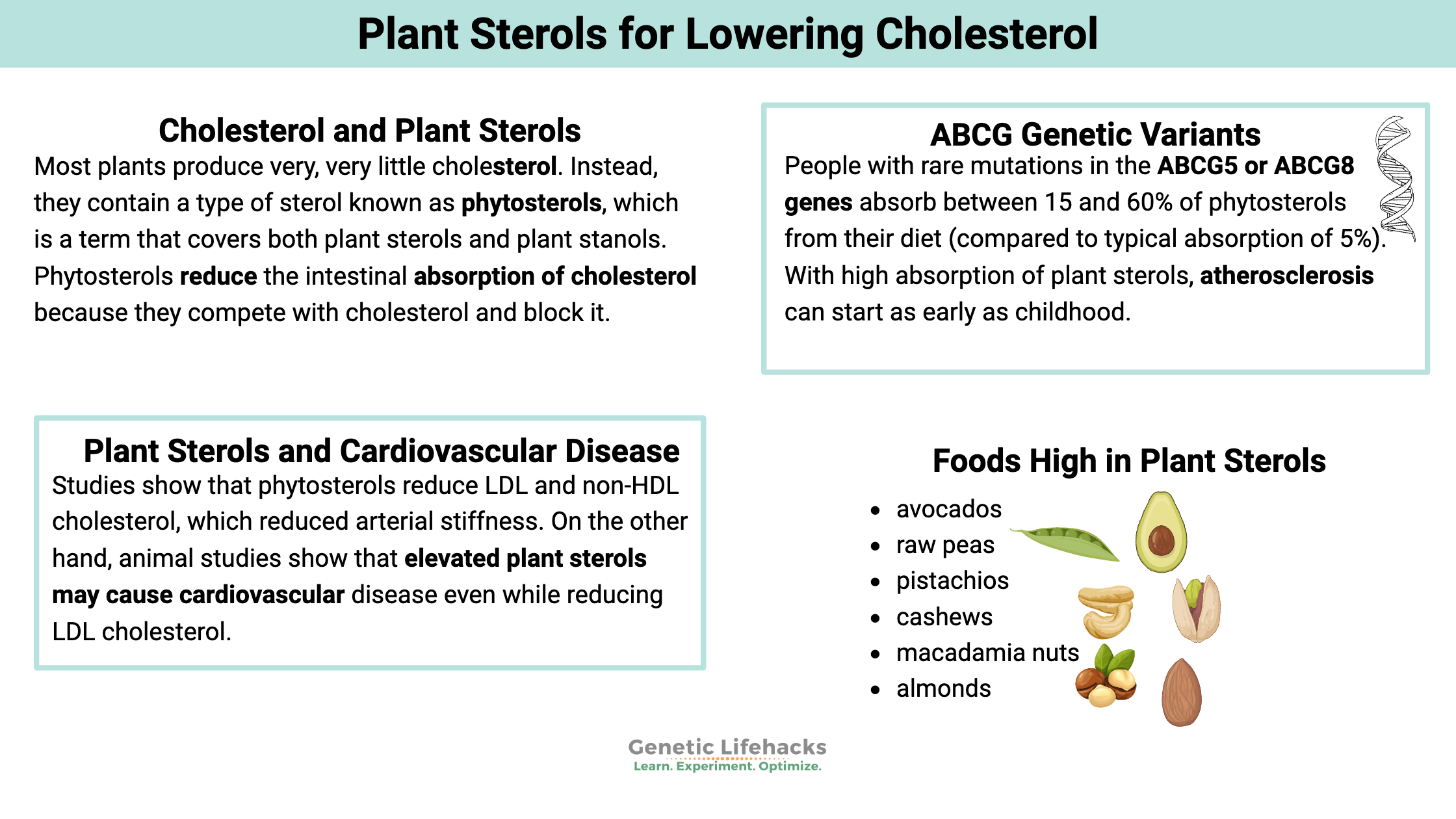
Cholesterol and Plant Sterols
Heart disease is the number one killer of people worldwide, and high cholesterol levels are a risk factor for heart disease. There are differing opinions about high cholesterol risks and the role of cholesterol in heart disease. Since research tends to support the link between high cholesterol levels and heart disease, stick with me here, and we can discuss the complexity later.
In general, high triglycerides and high LDL cholesterol levels are something that most doctors will worry about. Recommendations for dietary interventions often include limiting saturated fat and adding in plant sterols.[ref ![]() ] Your genetic variants may play a bigger role in whether plant sterols will work for you (and also how much of an impact saturated fat has, but that is another article).
] Your genetic variants may play a bigger role in whether plant sterols will work for you (and also how much of an impact saturated fat has, but that is another article).
Background on cholesterol:
Cholesterol is a general term for a type of lipid known as a sterol that is present in animal cells. There are several types of cholesterol made in the body, and you can also consume cholesterol in foods.
Cholesterol is transported in the blood attached to a lipoprotein – such as very-low-density lipoprotein (VLDL), low-density lipoprotein (LDL), high-density lipoprotein (HDL), and chylomicrons. LDL particles are the most common cholesterol carriers.
What does cholesterol do?
Cholesterol is used by all the cells in the body as part of the cell membrane. Within the cell membrane, cholesterol can stabilize the membrane, causing less fluidity in the phospholipid bilayer.
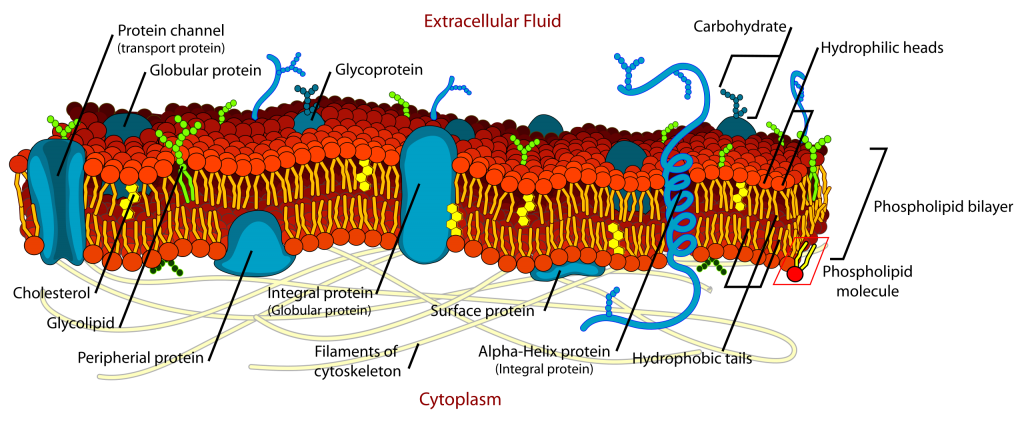
Detail of cell membrane. Cholesterol is shown in yellow. (Public domain image) Cholesterol is also a precursor molecule for vitamin D, bile acids, and steroid hormones. While often demonized as something ‘bad’, cholesterol is essential for your body to function.
Regulation of cholesterol:
In general, the body tightly regulates the level of cholesterol that is present at any given time. If you eat more cholesterol, your liver should make less of it. If you don’t eat many foods containing cholesterol, your body will increase cholesterol production.
Bile acids are created using cholesterol that is oxidized by the liver and then bound to glycine, taurine, or sulfate molecules. Your body uses bile acids to break down and digest fats from foods, and then the bile acids are mostly reabsorbed in the intestines and recycled. Some cholesterol, though, is lost each day via the excretion of bile acids through the colon.
Cholesterol from food:
Almost all of the cholesterol that you get via your diet is from animal-based foods. The cholesterol that you eat gets absorbed into the cells lining the small intestines, and people vary in how much cholesterol they absorb. There are a couple of different transporters involved in moving cholesterol from the intestinal cells. Plus, not all cholesterol from food ends up being absorbed and used by the body.[ref]
Plant sterols:
Most plants produce very, very little cholesterol.[ref] Instead, they contain a type of sterol known as phytosterols, which is a term that covers both plant sterols and plant stanols. Plant sterols, such as sitosterol, function similarly to cholesterol in the way that they regulate the fluidity of the cell membrane.
In general, people can absorb about 5% of dietary plant sterols. Phytosterols aren’t able to be used in humans (or other mammals).
It is estimated that people generally consume 200-400 mg/day of plant sterols, but that is going to vary widely depending on your diet (e.g., vegan vs. carnivore vs. mixed). A recent study found that vegans had the highest plant sterol intake and lowest cholesterol intake – and this was opposite from people eating an omnivore diet (low plant sterols, higher cholesterol). Interestingly, all the dietary pattern groups had similar blood cholesterol levels and sterol levels, showing that intake may not make much of a difference from the diet.[ref]
Plant sterols lower cholesterol levels:
Quite a few studies are showing in an average population group, increasing plant sterols will decrease cholesterol levels.
The cholesterol-lowering effect in an average population increases as the dose of plant sterols increases – up to about 2 -3g/day.[ref] An intake of around 2g/day of plant sterols is associated with an average decrease in LDL cholesterol of about 10%.[ref]
Phytosterols reduced the intestinal absorption of cholesterol because they compete with cholesterol and block it. It is thought that this lower intestinal absorption includes both dietary cholesterol and the recycling of cholesterol in bile acids.[ref]
Phytosterols have also been associated with a reduction in triglycerides in patients with high triglyceride levels.[ref]
Do plant sterols reduce cardiovascular disease?
That is the big question… and one that is not as well answered as I would like.
Some studies show that phytosterols reduce LDL and non-HDL cholesterol, which reduced arterial stiffness (important in cardiovascular health).[ref] Margarine that contains rapeseed-sterols (canola) reduced cholesterol levels and also reduced E-selectin concentrations, which is a cellular adhesion molecule important in the arteries and atherosclerosis.[ref]
A long-term study of plant sterol consumption (2.5 g/day for 85 weeks) showed that LDL cholesterol dropped, but this didn’t have a significant effect (positive or negative) on smaller blood vessel function. The study didn’t include very many participants in it, which would make getting a significant effect difficult.[ref]
Could plant sterols have the opposite effect and increase the risk of cardiovascular disease?
Something that you don’t see mentioned in the marketing literature for plant sterols is the link between increased atherosclerosis and an increased risk of heart disease for some people, depending on their genetic variants.
There are really rare genetic mutations that cause a condition known as sitosterolemia. People with rare mutations in the ABCG5 or ABCG8 genes absorb between 15 and 60% of phytosterols from their diet (compared with the normal 5% or so). The ABC genes code for proteins known as ATP-binding cassette transporters, which move substances – in this case, phytosterols – out of the cell. ABCG5 and ABCG8 code for the proteins that make up the sterolin transporter that pumps the absorbed plant sterols back into the intestines.[ref] These transporters may also be important in moving cholesterol back into the intestines as well.
So what happens with high absorption of plant sterols in sitosterolemia? Atherosclerosis can start as early as childhood, and some people develop xanthomas, which are yellowish growths that contain cholesterol. People with sitosterolemia can also have joint pain and hemolytic anemia.[ref]
While the negative effects of building up high amounts of plant sterols are clear, the question remains whether this is a spectrum… is there a point that a person without a rare genetic mutation can have negative effects from a higher intake of plant sterols?
A study came out about 10 years ago, showing that higher levels of sitosterol and campesterol (the most common phytosterols) were linked to an almost doubled risk of cardiovascular disease. The study participants all had a similar dietary intake of macronutrients as well as omega-6 fatty acid levels. The study concluded overall increased absorption (cholesterol, plant sterols) was associated with cardiovascular disease.[ref]
Several other studies also claim that the link between elevated plant sterols and coronary artery disease is due to overall cholesterol absorption and alterations to endogenous production.[ref]
On the other hand, animal studies show that elevated plant sterols (stigmasterols) cause cardiovascular disease even while reducing LDL cholesterol.[ref]
It could be that a specific type of plant sterol or oxidation of plant sterols is what elevates cardiovascular disease. Patients with higher oxidized plant sterol levels had an increase in ‘cardiovascular events’.[ref]
Overall, the FDA, European Food Safety Authority, and Health Canada have decided that food products with higher plant sterol levels can be labeled as being good for reducing cardiovascular disease.[ref] There was a nine-part study done that showed that plant sterol consumption is non-toxic and doesn’t cause cancer in animals.[ref](Studies done by Unilever, manufacturer of products with plant sterols)
Plant Sterols Genotype Report:
Members: Log in to see your data below.
Not a member? Join here.
Why is this section is now only for members? Here’s why…
Lifehacks:
There seemed to be a lot of assumptions and biases, such as industry sponsorship, in some of the studies on phytosterols. Keep this in mind whenever you’re reading research or articles on this topic.
Normal CYP7A1 benefits from plant sterols:
The research does seem to clearly show that for people with the normal CYP7A1 variant, increasing plant sterols to around 2g/day will decrease LDL cholesterol levels. If you were looking for a way to reduce LDL numbers before a blood test, this may work for you. The question, in my mind, is whether that decrease in LDL cholesterol makes a difference in cardiovascular disease risk (and whether long-term plant sterol supplementation would possibly increase CVD risk for some people).
Foods high in plant sterols:
Related Articles and Topics:
LDL Cholesterol
Heart disease is the leading cause of death in the US and around the world, and high LDL-cholesterol levels have been linked in many studies to increased heart disease. Standard medical advice on ideal cholesterol levels and cardiovascular disease is often confusing, ever-changing, and sometimes downright contradictory.
Lipoprotein(a): A big genetic risk for heart disease
By reading this information, you could possibly save your life today. This isn’t a scare tactic or overblown health-alert type of article – just statistics and solid genetics research on the increased risk of cardiovascular disease.
Sudden Cardiac Death and Hypertrophic Cardiomyopathy
Genetic mutations that cause hypertrophic cardiomyopathy can increase the risk of sudden cardiac death.
Neuropilins: Healthy blood vessels, lymphedema, Covid brain
Neuropilins act as receptors and are found on the surface of cells. Learn about its many roles body, such as in the immune, vascular and nervous systems.
References:
Alphonse, Peter A. S., and Peter J. H. Jones. “Revisiting Human Cholesterol Synthesis and Absorption: The Reciprocity Paradigm and Its Key Regulators.” Lipids, vol. 51, no. 5, May 2016, pp. 519–36. PubMed, https://doi.org/10.1007/s11745-015-4096-7.
Buch, Stephan, et al. “A Genome-Wide Association Scan Identifies the Hepatic Cholesterol Transporter ABCG8 as a Susceptibility Factor for Human Gallstone Disease.” Nature Genetics, vol. 39, no. 8, Aug. 2007, pp. 995–99. PubMed, https://doi.org/10.1038/ng2101.
Cabral, Carlos Eduardo, and Márcia Regina Simas Torres Klein. “Phytosterols in the Treatment of Hypercholesterolemia and Prevention
of Cardiovascular Diseases.” Arquivos Brasileiros de Cardiologia, vol. 109, no. 5, Nov. 2017, pp. 475–82. PubMed Central, https://doi.org/10.5935/abc.20170158.
Cederberg, Henna, et al. “Non-Cholesterol Sterol Levels Predict Hyperglycemia and Conversion to Type 2 Diabetes in Finnish Men.” PLoS ONE, vol. 8, no. 6, June 2013, p. e67406. PubMed Central, https://doi.org/10.1371/journal.pone.0067406.
Chupeerach, Chaowanee, et al. “Impact of Genetic Polymorphism on LDL-C Response to Plant Stanol Ester Intake.” Journal of the Medical Association of Thailand = Chotmaihet Thangphaet, vol. 99, no. 6, June 2016, pp. 723–31.
Consortium, The IBC 50K CAD. “Large-Scale Gene-Centric Analysis Identifies Novel Variants for Coronary Artery Disease.” PLOS Genetics, vol. 7, no. 9, Sept. 2011, p. e1002260. PLoS Journals, https://doi.org/10.1371/journal.pgen.1002260.
Dumolt, Jerad H., and Todd C. Rideout. “The Lipid-Lowering Effects and Associated Mechanisms of Dietary Phytosterol Supplementation.” Current Pharmaceutical Design, vol. 23, no. 34, 2017, pp. 5077–85. PubMed Central, https://doi.org/10.2174/1381612823666170725142337.
Fuhrmann, Arne, et al. “Plasma Levels of the Oxyphytosterol 7α-Hydroxycampesterol Are Associated with Cardiovascular Events.” Atherosclerosis, vol. 279, Dec. 2018, pp. 17–22. PubMed, https://doi.org/10.1016/j.atherosclerosis.2018.10.010.
Gylling, Helena, Janne Halonen, et al. “The Effects of Plant Stanol Ester Consumption on Arterial Stiffness and Endothelial Function in Adults: A Randomised Controlled Clinical Trial.” BMC Cardiovascular Disorders, vol. 13, July 2013, p. 50. PubMed Central, https://doi.org/10.1186/1471-2261-13-50.
Gylling, Helena, Maarit Hallikainen, et al. “The Metabolism of Plant Sterols Is Disturbed in Postmenopausal Women with Coronary Artery Disease.” Metabolism: Clinical and Experimental, vol. 58, no. 3, Mar. 2009, pp. 401–07. PubMed, https://doi.org/10.1016/j.metabol.2008.10.015.
Heggen, Eli, et al. “Effects of Margarine Enriched with Plant Sterol Esters from Rapeseed and Tall Oils on Markers of Endothelial Function, Inflammation and Hemostasis.” Scandinavian Journal of Clinical and Laboratory Investigation, vol. 75, no. 2, Apr. 2015, pp. 189–92. PubMed, https://doi.org/10.3109/00365513.2014.992040.
Hepburn, P. A., et al. “Safety Evaluation of Phytosterol Esters. Part 2. Subchronic 90-Day Oral Toxicity Study on Phytosterol Esters–a Novel Functional Food.” Food and Chemical Toxicology: An International Journal Published for the British Industrial Biological Research Association, vol. 37, no. 5, May 1999, pp. 521–32. PubMed, https://doi.org/10.1016/s0278-6915(99)00030-7.
Jaceldo-Siegl, Karen, et al. “Variations in Dietary Intake and Plasma Concentration of Plant Sterols across Plant-Based Diets among North American Adults.” Molecular Nutrition & Food Research, vol. 61, no. 8, Aug. 2017, p. 10.1002/mnfr.201600828. PubMed Central, https://doi.org/10.1002/mnfr.201600828.
Kelly, Elton R., et al. “Effects of Long Term Plant Sterol and -Stanol Consumption on the Retinal Vasculature: A Randomized Controlled Trial in Statin Users.” Atherosclerosis, vol. 214, no. 1, Jan. 2011, pp. 225–30. PubMed, https://doi.org/10.1016/j.atherosclerosis.2010.10.038.
Mackay, Dylan S., et al. “Cholesterol Ester Transfer Protein Polymorphism Rs5882 Is Associated with Triglyceride-Lowering in Response to Plant Sterol Consumption.” Applied Physiology, Nutrition, and Metabolism = Physiologie Appliquee, Nutrition Et Metabolisme, vol. 40, no. 8, Aug. 2015, pp. 846–49. PubMed, https://doi.org/10.1139/apnm-2015-0039.
MacKay, Dylan S., et al. “CYP7A1-Rs3808607 and APOE Isoform Associate with LDL Cholesterol Lowering after Plant Sterol Consumption in a Randomized Clinical Trial.” The American Journal of Clinical Nutrition, vol. 102, no. 4, Oct. 2015, pp. 951–57. PubMed, https://doi.org/10.3945/ajcn.115.109231.
Matthan, Nirupa R., et al. “Alterations in Cholesterol Absorption/Synthesis Markers Characterize Framingham Offspring Study Participants with CHD [S].” Journal of Lipid Research, vol. 50, no. 9, Sept. 2009, pp. 1927–35. www.jlr.org, https://doi.org/10.1194/jlr.P900039-JLR200.
Mo, Shunyan, et al. “Quantitative Analysis of Phytosterols in Edible Oils Using APCI Liquid Chromatography-Tandem Mass Spectrometry.” Lipids, vol. 48, no. 9, Sept. 2013, pp. 949–56. PubMed Central, https://doi.org/10.1007/s11745-013-3813-3.
Patel, Shailendra B., et al. “ABCG5 and ABCG8: More than a Defense against Xenosterols.” Journal of Lipid Research, vol. 59, no. 7, July 2018, pp. 1103–13. PubMed Central, https://doi.org/10.1194/jlr.R084244.
“Phytosterols.” Linus Pauling Institute, 29 Apr. 2014, https://lpi.oregonstate.edu/mic/dietary-factors/phytochemicals/phytosterols.
Piironen, Vieno, et al. “Plant Sterols in Vegetables, Fruits and Berries: Plant Sterols in Vegetables, Fruits and Berries.” Journal of the Science of Food and Agriculture, vol. 83, no. 4, Mar. 2003, pp. 330–37. DOI.org (Crossref), https://doi.org/10.1002/jsfa.1316.
Ras, Rouyanne T., et al. “LDL-Cholesterol-Lowering Effect of Plant Sterols and Stanols across Different Ranges: A Meta-Analysis of Randomised Controlled Studies.” The British Journal of Nutrition, vol. 112, no. 2, July 2014, pp. 214–19. PubMed Central, https://doi.org/10.1017/S0007114514000750.
San Mauro Martín, Ismael, et al. “Gene Influence in the Effectiveness of Plant Sterols Treatment in Children: Pilot Interventional Study.” Nutrients, vol. 11, no. 10, Oct. 2019, p. 2538. PubMed Central, https://doi.org/10.3390/nu11102538.
Silbernagel, Günther, et al. “High Intestinal Cholesterol Absorption Is Associated With Cardiovascular Disease and Risk Alleles in ABCG8 and ABO: Evidence From the LURIC and YFS Cohorts and From a Meta-Analysis.” Journal of the American College of Cardiology, vol. 62, no. 4, July 2013, pp. 291–99. ScienceDirect, https://doi.org/10.1016/j.jacc.2013.01.100.
Sitosterolemia: MedlinePlus Genetics. https://medlineplus.gov/genetics/condition/sitosterolemia/. Accessed 19 Oct. 2022.
Sonawane, Prashant D., et al. “Plant Cholesterol Biosynthetic Pathway Overlaps with Phytosterol Metabolism.” Nature Plants, vol. 3, no. 1, Dec. 2016, pp. 1–13. www.nature.com, https://doi.org/10.1038/nplants.2016.205.
Srivastava, Anshika, Naveen Garg, et al. “Effect of Genetic Variant (Rs11887534) in ABCG8 Gene in Coronary Artery Disease and Response to Atorvastatin Therapy.” Disease Markers, vol. 28, no. 5, 2010, pp. 307–13. PubMed, https://doi.org/10.3233/DMA-2010-0710.
Srivastava, Anshika, Anvesha Srivastava, et al. “Role of ABCG8 D19H (Rs11887534) Variant in Gallstone Susceptibility in Northern India.” Journal of Gastroenterology and Hepatology, vol. 25, no. 11, Nov. 2010, pp. 1758–62. PubMed, https://doi.org/10.1111/j.1440-1746.2010.06349.x.
Tao, Caroline, et al. “Stigmasterol Accumulation Causes Cardiac Injury and Promotes Mortality.” Communications Biology, vol. 2, 2019, p. 20. PubMed, https://doi.org/10.1038/s42003-018-0245-x.
Teupser, Daniel, et al. “Genetic Regulation of Serum Phytosterol Levels and Risk of Coronary Artery Disease.” Circulation: Cardiovascular Genetics, vol. 3, no. 4, Aug. 2010, pp. 331–39. ahajournals.org (Atypon), https://doi.org/10.1161/CIRCGENETICS.109.907873.
VCV000004967.22 – ClinVar – NCBI. https://www.ncbi.nlm.nih.gov/clinvar/variation/4967/. Accessed 19 Oct. 2022.
VCV000004976.9 – ClinVar – NCBI. https://www.ncbi.nlm.nih.gov/clinvar/variation/4976/. Accessed 19 Oct. 2022.
Wu, Ge, et al. “ABCG5/8 Variants Are Associated with Susceptibility to Coronary Heart Disease.” Molecular Medicine Reports, vol. 9, no. 6, June 2014, pp. 2512–20. PubMed, https://doi.org/10.3892/mmr.2014.2098.