Key takeaways:
~ Polycythemia vera is a slow, chronic overproduction of blood cells caused by somatic mutations in the JAK2 gene.
~ The overproduction of cells causes the blood to thicken, increasing the risk of clots or an enlarged spleen.
~ While the JAK2 mutation usually arises later in life, inherited genetic variants can increase your susceptibility to it.
What is polycythemia vera?
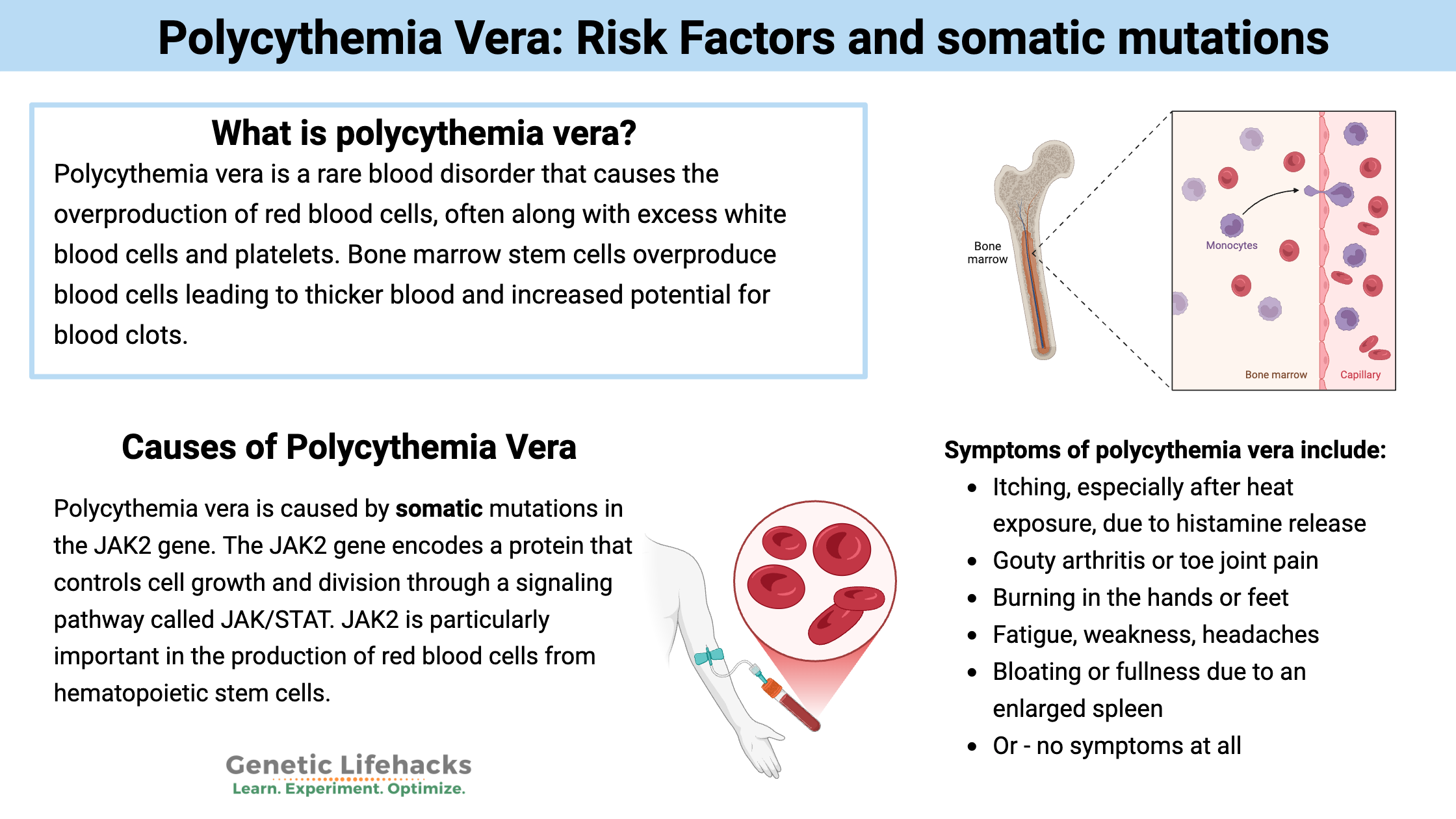
Polycythemia vera is a rare blood disorder that causes the overproduction of red blood cells, often along with excess white blood cells and platelets. It is usually caused by a somatic mutation in the JAK2 gene, which causes the bone marrow to overproduce blood cells.
The excess blood cells can cause the blood to thicken, leading to a variety of vague symptoms, an increased risk of blood clots, and sometimes an enlarged spleen. The condition is usually first suspected because of high hemoglobin or blood cell counts, and is usually confirmed with genetic testing. It is more commonly found in people over age 60, with a prevalence of about 2-5 in 10,000 people.[ref][ref]
Symptoms of polycythemia vera can include:[ref]
- Itching, especially after heat exposure, due to histamine release
- Gouty arthritis or toe joint pain
- Burning in the hands or feet
- Fatigue, weakness, headaches
- Bloating or fullness due to an enlarged spleen
However, many people with polycythemia vera (up to 50% according to one study) have no symptoms when they are diagnosed. Instead, it is discovered based on blood test results.[ref]
While hemoglobin and red blood cell counts are usually high, iron deficiency or altered iron levels are often a part of polycythemia vera.[ref]
What causes polycythemia vera?
Polycythemia vera is a chronic, progressive condition that is considered a myeloproliferative neoplasm that affects the blood-forming cells in the bone marrow. It’s not a quick overperliferation of cells, like many types of cancer, but instead causes symptoms for years. The survival rate in younger patients is more than 35 years.[ref]
Blood tests showing elevated hemoglobin and hematocrit levels are often the first sign. The World Health Organization diagnostic thresholds for polycythemia vera are 16.5 g/dL (hemoglobin)/49% (hematocrit) for men and 16 g/dL/48% for women. This may vary slightly with altitude, as people living at higher altitudes tend to have higher hematocrit values.
Polycythemia vera is caused by somatic mutations in the JAK2 gene. There are other genetic factors involved as well, but a JAK2 mutation is necessary.
The JAK2 gene encodes a protein that controls cell growth and division through a signaling pathway called JAK/STAT. JAK2 is particularly important in the production of red blood cells from hematopoietic stem cells (bone marrow stem cells)[ref] While over 95% of people with polycythemia vera have JAK2 mutations, the same mutations are also found in a smaller percentage of people with leukemia or other blood cancers. Thus, the same mutation can cause different responses in individuals.[ref][ref]
Somatic vs. Germline Mutations:
Let me give you some context about mutations – skip ahead if you know this.
In genetics, germline mutations are the changes in your DNA that you’re born with. These are the inherited changes that are present in all of your cells from birth. Germline refers to being present in the egg or sperm (gametes).
- Germline (inherited) mutations cause genetic diseases such as cystic fibrosis or sickle cell anemia.
Somatic refers to the rest of the body (not the gametes). Somatic mutations occur in cells in the body as they replicate. They are not something you pass on to your children or inherit from your parents.
- An example of a somatic mutation is one that occurs in cancer.
In the case of polycythemia vera, the somatic mutation occurs at some point in life in the hematopoietic cells in the bone marrow that produce blood cells.
JAK2 Somatic Mutations Cause Polycythemia Vera
Polycythemia vera is caused by a gain-of-function mutation in the JAK2 (Janus kinase–signal transducer) gene. The most common mutation in JAK2 that causes polycythemia vera is called V617F. A less common cause is a mutation in exon 12 of the gene. Again, these are mutations that occur in cells at some point in your life and aren’t covered by direct-to-consumer genetic tests like 23andMe or AncestryDNA.
Interestingly, recent research shows that the expansion of cells that carry the JAK2 mutation happens over the course of several years. This isn’t a quick cancer growth, but rather a slower change that gets incorporated over time.[ref][ref]
Germline genetic variants that increase susceptibility to polycythemia Vera:
While the cause of JAK2 mutations in polycythemia vera is usually a somatic mutation, researchers have found that it tends to run in families. People who have a first-degree relative (parent, sibling) with polycythemia vera have an increased risk of developing it.
A study in Sweden found that first-degree relatives had a 5 to 7-fold higher relative risk of polycythemia vera compared to people without a parent or sibling with the disease.[ref]
This shows that inherited genes can also play a role in susceptibility. It is likely that this also combines with environmental factors because relatives often are exposed to the same environment.
Genetic variants that you’re born with can increase the susceptibility to polycythemia vera in a couple of ways:
- Recent research shows that common inherited variants can increase the susceptibility to having a JAK2 somatic mutation.[ref] These common JAK2 changes make it slightly more likely that a mutation can arise in the gene. (In the genotype report section below.)
- Variants in cancer suppressor genes that increase the relative risk of several types of cancer also increase susceptibility to polycythemia vera.
Idiopathic Erythrocytosis:
What happens if someone has all the symptoms of polycythemia vera but doesn’t have a JAK2 somatic mutation? That is usually referred to as “idiopathic erythrocytosis,” meaning a high blood cell count with unknown origin. About 5% of patients thought to have polycythemia vera don’t have a JAK2 mutation. [ref]
Recent studies have shown that both inherited (germline) mutations and somatic mutations in genes other than JAK2 can cause idiopathic erythrocytosis.[ref]
What causes somatic JAK2 mutations?
This is a hard question to answer definitively. Mutations occur all the time when cells replicate, but almost all errors get caught and fixed by DNA repair processes. Age is the greatest risk factor for polycythemia vera and blood cancers because you will simply have more mutations and chances for mutations to slip through the error checks over time.
However, there are changes that occur with age that are part of the increased risk of JAK2 mutations, and there are some environmental factors that may also contribute.
- An increase in oxidative stress or ROS in the bone marrow cells can increase the risk of polycythemia vera.
- MicroRNAs are small RNA strands that can alter gene expression. In people with polycythemia vera, researchers have found that a specific miRNA, called miR-451, is upregulated. When they inhibit that miRNA in animals, they can prevent the overaccumulation of red blood cells.[ref]
- Gender-based discrepancies in the susceptibility of polycythemia vera point to a role for the inactivation of the X chromosome changing during aging.[ref]
Genotype report: Polycythemia vera susceptibility
Just to reiterate – the data that you get from a genetic test, such as 23andMe, AncestryDNA, or even whole genome sequencing, is going to show the genes that you were born with and not somatic mutations that arise.
Polycythemia vera is usually caused by a mutation that arises in your bone marrow cells (somatic mutation).
However, genetic variants that you are born with can increase the susceptibility to forming a JAK2 mutation later in life. This information is relevant for someone who has a 1st degree relative who has polycythemia vera, but it isn’t predictive of getting this rare condition.
Lifehacks:
Treatment for polycythemia vera may include phlebotomy (removal of excess red blood cells), medications to reduce red blood cell production, and anticoagulants, such as aspirin, to prevent blood clots. In some cases, more advanced treatments, such as targeted therapies or stem cell transplantation, may be considered.[ref]
What can you do if you have the risk alleles for polycythemia vera?
Talk with your doctor if you have a first-degree relative with polycythemia vera about whether testing is warranted. Your doctor may be able to help you with devising a plan for prevention.
Related articles and topics: