Key takeaways:
~ PPARδ is a key player in how and when your muscles burn fat for fuel.
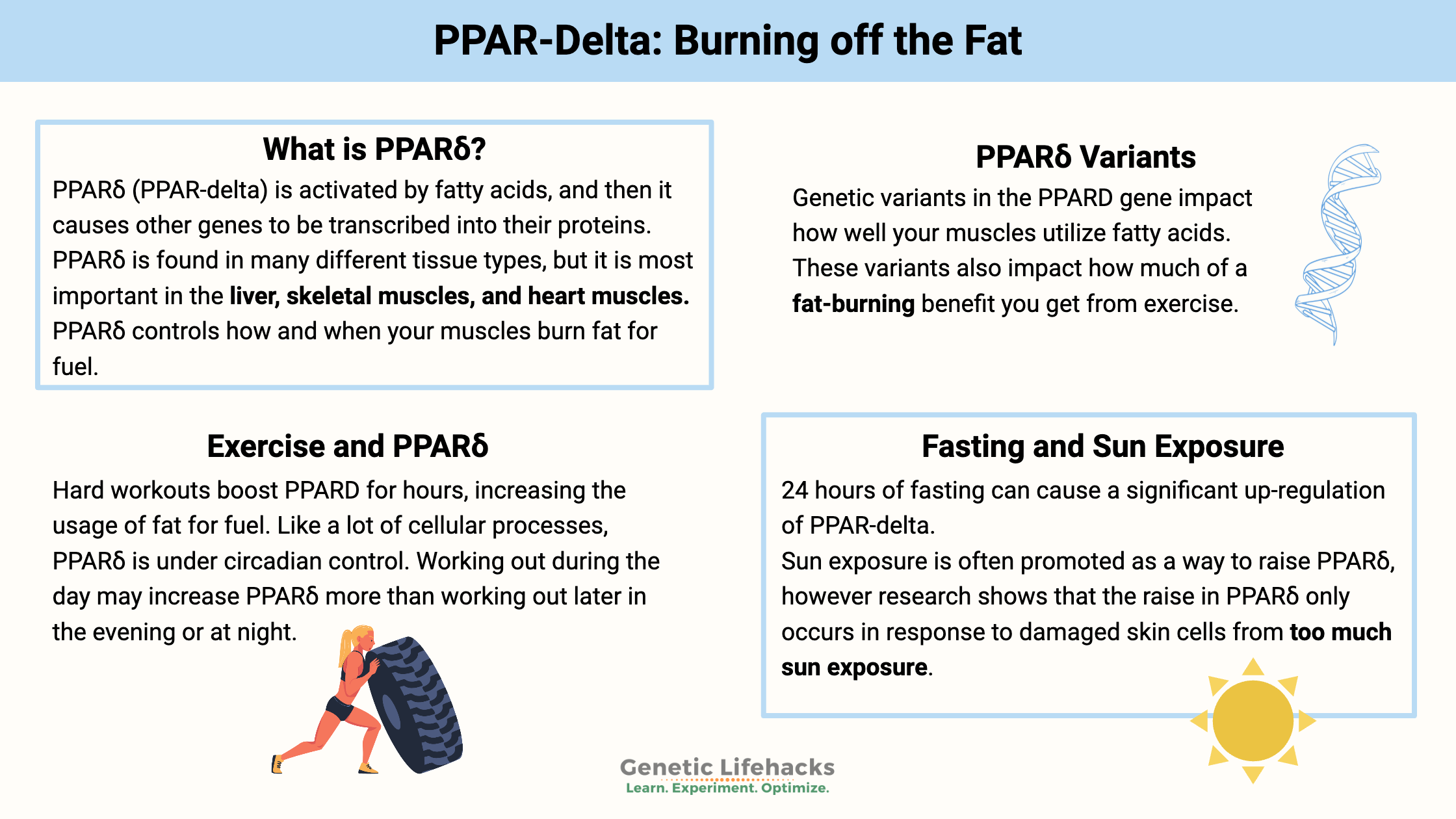
~Genetic variants in the PPARD gene impact how well your muscles utilize fatty acids. These variants also impact how much of a fat-burning benefit you get from exercise.[ref]
PPARδ: Fat burning and exercise response
PPARδ (PPAR-delta) is part of the PPAR family of receptors. These receptors are found in the nucleus of the cell, surrounding certain areas of the DNA. PPARδ is activated by fatty acids, and then it causes other genes to be transcribed into their proteins.
Essentially, PPARδ is a sensor for cellular metabolism, switching on the genes needed for burning fat instead of glucose.
PPARδ is found in many different tissue types, but it is most important in the liver, skeletal muscles, and heart muscles.
In the skeletal muscles, PPARδ is important in using fatty acids for fuel and how muscles respond to exercise.[ref]
In the liver, PPARδ increases the use of fat for fuel, and it is thus protective against fatty liver disease.[ref]
Increased levels of PPARδ are linked to less fat in the heart muscles and better uptake of glucose and fatty acids in the skeletal muscles. Increased levels of PPAR-delta can also lead to decreased cholesterol absorption in the intestines.[ref]
There are a number of different long-chain fatty acids that can bind to and activate PPARδ, produced in the body, or from foods. Common fatty acids from foods include polyunsaturated fats such as arachidonic acid and linoleic acid.[ref]
PPARδ in weight loss and exercise training:
There are different goals for exercising and training – and PPAR-delta influences how easily you can reach those goals.
Some people work out to lose weight; others train to increase muscle mass. For some, exercise gives greater cardiovascular health benefits; for others, it can raise (or lower) cholesterol levels.
PPARδ acts as an energy manager for endurance exercise – switching the muscles to burning fat and preserving some glucose. Animal studies show that stimulating PPAR-delta using drugs that bind to it can extend running time significantly. Research shows that it does this by using fatty acids for fuel and sparing glucose to be used as needed.[ref]
The PPARD gene codes for PPARδ. Genetic variants in the PPARD gene influence how exercise impacts weight loss, strength gains, cholesterol levels, and cardiovascular health benefits – often in opposite ways.
It is not as simple as “this is a good genetic variant” for PPARD. There are trade-offs, and your view of the variants may depend on your goals.
PPAR-delta and Muscle Fiber Type:
There are two main categories for muscle fiber type: type 1 (slow) and type 2 (fast-twitch). Type I muscle fibers are used more in endurance athletes (long-distance runners), and type 2, or fast-twitch muscle fibers, are important for a burst of speed such as in sprinting or powerlifting.
In animal studies, activating PPARδ causes a switch to forming more type 1, slow-twitch muscle fibers.[ref]
PPAR-delta is anti-inflammatory:
In general, increasing PPARδ can tamp down an overactive inflammatory response.
In a cell culture of heart tissue, increasing PPARδ caused a decrease in the production of the inflammatory cytokine TNF-alpha. In cells created without the PPAR-delta gene, the addition of a bacterial inflammatory molecule causes exaggerated TNF-alpha production (not good).[ref]
Your muscles accumulate tissue damage when you work out – or just through everyday life. Activating PPAR-delta, in turn, activates FOXA2, which tamps down the inflammatory response to tissue damage. Studies are now looking at drugs that activate PPAR-delta as a way of combating muscular pain disorders.[ref]
Can you influence PPAR-delta with fat intake?
Research from the 90s shows that a high-fat diet may increase overall metabolism in the muscles through increasing mitochondrial fatty acid oxidation.
Quick science refresher: Your mitochondria (the powerhouse of the cell :-) turn fat or sugar into energy in the form of ATP. Cells have hundreds to thousands of mitochondria, processing fuel and turning it into energy. More mitochondria, therefore, increases using up fat or sugar and causes an increase in energy.
Studies in rats show that increasing long-chain fatty acids increases mitochondrial fatty acid oxidation in the skeletal muscles. This is thought to be due to the increase in PPAR-delta.[ref]
Medium-chain fatty acids may not be the way to go, though. Animal studies also show that coconut oil, high in medium-chain fatty acids, inhibits PPARδ.[ref]
PPARD in cancer:
Studies show that PPARδ is upregulated in cancer cells, increasing the formation of new blood vessels for the tumors. Blocking PPARD represses metastasis.[ref][ref]
The PPARδ agonist known as GW-501 has been shown in cell studies and animal studies to promote tumorigenesis. Activating the PPAR-delta receptor in breast cancer cells also increases the spread of cancer. On the other hand, some studies show that PPAR-delta is downregulated in prostate cancer. Additionally, the topical application of a PPAR-delta agonist has been shown to delay chemical-induced skin cancer.[ref]
PPARδ in the brain:
In addition to its role in fatty acid metabolism in muscles, PPARδ is found abundantly in the brain, where it is neuroprotective.[ref]
People with Huntington’s disease, a progressive, genetic neurodegenerative disease, have low levels of PPARδ in the neurons. Animal studies show that specifically targeting neurons with certain PPARδ activators can reverse some of the neurodegenerative effects of Huntington’s.[ref][ref]
In animal models of depression, low brain levels of PPARδ are linked with chronic mild stress and learned helplessness. Increasing the brain PPARδ prevented depression-like behaviors.[ref]
PPARD Genotype Report:
Access this content:
An active subscription is required to access this content.
Lifehacks for increasing PPARδ:
Exercise:
A great way to boost PPARD in muscles is through exercise. Research shows that hard workouts boost PPARD for hours, increasing the usage of fat for fuel.[ref]
As you can see from the PPARD genetic variants above, we don’t all get the same ‘bang for your buck’ with exercise. But… don’t let this be an excuse for you.
Exercise is good for (almost) everyone. So whether or not you get as much cardiovascular benefit from exercise as others do – you will still get some benefit. It may be that you just need to work out a little more often – or a little longer – than other people to get the same benefits.
Timing matters:
Like a lot of cellular processes, PPARδ is under circadian control. The body’s core molecular clock relies on increased levels of certain molecules (CLOCK, BMAL1) during the day, and then at night, a couple of other molecules (CRY and PER) rule the dark.
A recent study showed that CRY1 and CRY2 (circadian clock molecules that are activated at night) repress some of the target genes turned on by PPARδ.[ref]
Thus, if you are looking for exercise benefits due to boosting PPARδ, working out during the day may be better than working out later in the evening or at night.
Fasting:
In cell studies, 24 hours of fasting caused a significant up-regulation of PPAR-delta.[ref]
Sun exposure:
Other websites suggest that you can increase PPARδ by sun exposure, but reading the referenced studies paints a different picture. UVB radiation that causes damage to skin cells does eventually increase PPAR-delta in those cells. This increase is thought to counteract the inflammatory process that is going on in wound healing due to the damage from overexposure to UVB.[ref] Getting some sunshine each day is great – but you don’t want too much sun, causing skin damage to raise the PPARδ.
Supplements and Peptides that affect PPAR-delta:
Access this content:
An active subscription is required to access this content.
Related Articles and Topics:
References:
Amengual, Jaume, et al. “Retinoic Acid Increases Fatty Acid Oxidation and Irisin Expression in Skeletal Muscle Cells and Impacts Irisin In Vivo.” Cellular Physiology and Biochemistry: International Journal of Experimental Cellular Physiology, Biochemistry, and Pharmacology, vol. 46, no. 1, 2018, pp. 187–202. PubMed, doi:10.1159/000488422.
Burch, Lindsay R., et al. “Peroxisome Proliferator-Activated Receptor-Delta Genotype Influences Metabolic Phenotype and May Influence Lipid Response to Statin Therapy in Humans: A Genetics of Diabetes Audit and Research Tayside Study.” The Journal of Clinical Endocrinology and Metabolism, vol. 95, no. 4, Apr. 2010, pp. 1830–37. PubMed, doi:10.1210/jc.2009-1201.
Cao, Yixuan, et al. “Polymorphism of the PPARD Gene and Dynamic Balance Performance in Han Chinese Children.” Hereditas, vol. 156, May 2019. PubMed Central, doi:10.1186/s41065-019-0092-x.
d’Angelo, Michele, et al. “Lifestyle and Food Habits Impact on Chronic Diseases: Roles of PPARs.” International Journal of Molecular Sciences, vol. 20, no. 21, Oct. 2019. PubMed Central, doi:10.3390/ijms20215422.
Dickey, Audrey S., Dafne N. Sanchez, et al. “PPARδ Activation by Bexarotene Promotes Neuroprotection by Restoring Bioenergetic and Quality Control Homeostasis.” Science Translational Medicine, vol. 9, no. 419, Dec. 2017. PubMed, doi:10.1126/scitranslmed.aal2332.
Dickey, Audrey S., Victor V. Pineda, et al. “PPARδ Repression in Huntington’s Disease and Its Essential Role in CNS Translate into a Potent Agonist Therapy.” Nature Medicine, vol. 22, no. 1, Jan. 2016, pp. 37–45. PubMed Central, doi:10.1038/nm.4003.
Ding, Guoliang, et al. “PPARdelta Modulates Lipopolysaccharide-Induced TNFalpha Inflammation Signaling in Cultured Cardiomyocytes.” Journal of Molecular and Cellular Cardiology, vol. 40, no. 6, June 2006, pp. 821–28. PubMed, doi:10.1016/j.yjmcc.2006.03.422.
Domańska-Senderowska, D., et al. “Analysis of the PPARD Gene Expression Level Changes in Football Players in Response to the Training Cycle.” Balkan Journal of Medical Genetics: BJMG, vol. 21, no. 1, June 2018, pp. 19–25. PubMed, doi:10.2478/bjmg-2018-0008.
Fan, Weiwei, et al. “PPARδ Promotes Running Endurance by Preserving Glucose.” Cell Metabolism, vol. 25, no. 5, May 2017, pp. 1186-1193.e4. PubMed Central, doi:10.1016/j.cmet.2017.04.006.
Garcia-Roves, Pablo, et al. “Raising Plasma Fatty Acid Concentration Induces Increased Biogenesis of Mitochondria in Skeletal Muscle.” Proceedings of the National Academy of Sciences of the United States of America, vol. 104, no. 25, June 2007, pp. 10709–13. PubMed Central, doi:10.1073/pnas.0704024104.
Gill, Navneet, et al. “Anti-Inflammatory and Anti-Hyperalgesic Effect of All-Trans Retinoic Acid in Carrageenan-Induced Paw Edema in Wistar Rats: Involvement of Peroxisome Proliferator-Activated Receptor-β/δ Receptors.” Indian Journal of Pharmacology, vol. 45, no. 3, June 2013, pp. 278–82. PubMed, doi:10.4103/0253-7613.111944.
Hautala, Arto J., et al. “Peroxisome Proliferator-Activated Receptor-Delta Polymorphisms Are Associated with Physical Performance and Plasma Lipids: The HERITAGE Family Study.” American Journal of Physiology. Heart and Circulatory Physiology, vol. 292, no. 5, May 2007, pp. H2498-2505. PubMed, doi:10.1152/ajpheart.01092.2006.
Holst, Dorte, et al. “Nutritional Regulation and Role of Peroxisome Proliferator-Activated Receptor Delta in Fatty Acid Catabolism in Skeletal Muscle.” Biochimica Et Biophysica Acta, vol. 1633, no. 1, July 2003, pp. 43–50. PubMed, doi:10.1016/s1388-1981(03)00071-4.
Ji, Miao-Jin, et al. “Hippocampal PPARδ Overexpression or Activation Represses Stress-Induced Depressive Behaviors and Enhances Neurogenesis.” International Journal of Neuropsychopharmacology, vol. 19, no. 1, Sept. 2015. PubMed Central, doi:10.1093/ijnp/pyv083.
Jordan, Sabine D., et al. “CRY1/2 Selectively Repress PPARδ and Limit Exercise Capacity.” Cell Metabolism, vol. 26, no. 1, July 2017, pp. 243-255.e6. www.cell.com, doi:10.1016/j.cmet.2017.06.002.
Komiya, Yusuke, et al. “Increase in Muscle Endurance in Mice by Dietary Yamabushitake Mushroom (Hericium Erinaceus) Possibly via Activation of PPARδ.” Animal Science Journal = Nihon Chikusan Gakkaiho, vol. 90, no. 6, June 2019, pp. 781–89. PubMed Central, doi:10.1111/asj.13199.
Leońska-Duniec, Agata, et al. “The Polymorphisms of the PPARD Gene Modify Post-Training Body Mass and Biochemical Parameter Changes in Women.” PLOS ONE, vol. 13, no. 8, Aug. 2018, p. e0202557. PLoS Journals, doi:10.1371/journal.pone.0202557.
Liu, Yi, Yasunori Deguchi, et al. “Pleiotropic Effects of PPARD Accelerate Colorectal Tumorigenesis, Progression, and Invasion.” Cancer Research, vol. 79, no. 5, 01 2019, pp. 954–69. PubMed, doi:10.1158/0008-5472.CAN-18-1790.
Liu, Yi, Jennifer K. Colby, et al. “The Role of PPAR-δ in Metabolism, Inflammation, and Cancer: Many Characters of a Critical Transcription Factor.” International Journal of Molecular Sciences, vol. 19, no. 11, Oct. 2018. PubMed Central, doi:10.3390/ijms19113339.
Manio, Mark Christian, et al. “Low-Fat Diet, and Medium-Fat Diets Containing Coconut Oil and Soybean Oil Exert Different Metabolic Effects in Untrained and Treadmill-Trained Mice.” Journal of the International Society of Sports Nutrition, vol. 15, no. 1, June 2018, p. 29. PubMed, doi:10.1186/s12970-018-0234-y.
Petr, Miroslav, et al. “The Role of Peroxisome Proliferator-Activated Receptors and Their Transcriptional Coactivators Gene Variations in Human Trainability: A Systematic Review.” International Journal of Molecular Sciences, vol. 19, no. 5, May 2018. PubMed Central, doi:10.3390/ijms19051472.
Phua, Wendy Wen Ting, et al. “PPARβ/δ Agonism Upregulates Forkhead Box A2 to Reduce Inflammation in C2C12 Myoblasts and in Skeletal Muscle.” International Journal of Molecular Sciences, vol. 21, no. 5, Mar. 2020. PubMed, doi:10.3390/ijms21051747.
Sertznig, Pit, and Jörg Reichrath. “Peroxisome Proliferator-Activated Receptors (PPARs) in Dermatology.” Dermato-Endocrinology, vol. 3, no. 3, 2011, pp. 130–35. PubMed Central, doi:10.4161/derm.3.3.15025.
Stefan, Norbert, et al. “Genetic Variations in PPARD and PPARGC1A Determine Mitochondrial Function and Change in Aerobic Physical Fitness and Insulin Sensitivity during Lifestyle Intervention.” The Journal of Clinical Endocrinology and Metabolism, vol. 92, no. 5, May 2007, pp. 1827–33. PubMed, doi:10.1210/jc.2006-1785.
Tang, Lizhi, et al. “PPARD Rs2016520 Polymorphism Is Associated with Metabolic Traits in a Large Population of Chinese Adults.” Gene, vol. 585, no. 2, July 2016, pp. 191–95. PubMed, doi:10.1016/j.gene.2016.02.035.
—. “PPARD Rs2016520 Polymorphism Is Associated with Metabolic Traits in a Large Population of Chinese Adults.” Gene, vol. 585, no. 2, July 2016, pp. 191–95. PubMed, doi:10.1016/j.gene.2016.02.035.
Thamer, Claus, et al. “Variations in PPARD Determine the Change in Body Composition during Lifestyle Intervention: A Whole-Body Magnetic Resonance Study.” The Journal of Clinical Endocrinology and Metabolism, vol. 93, no. 4, Apr. 2008, pp. 1497–500. PubMed, doi:10.1210/jc.2007-1209.
—. “Variations in PPARD Determine the Change in Body Composition during Lifestyle Intervention: A Whole-Body Magnetic Resonance Study.” The Journal of Clinical Endocrinology and Metabolism, vol. 93, no. 4, Apr. 2008, pp. 1497–500. PubMed, doi:10.1210/jc.2007-1209.
Tong, Lei, et al. “PPARδ Attenuates Hepatic Steatosis through Autophagy-Mediated Fatty Acid Oxidation.” Cell Death & Disease, vol. 10, no. 3, Feb. 2019. PubMed Central, doi:10.1038/s41419-019-1458-8.
Wagner, Nicole, and Kay-Dietrich Wagner. “PPAR Beta/Delta and the Hallmarks of Cancer.” Cells, vol. 9, no. 5, May 2020. PubMed Central, doi:10.3390/cells9051133.
Wang, Yong-Xu, et al. “Regulation of Muscle Fiber Type and Running Endurance by PPARδ.” PLoS Biology, vol. 2, no. 10, Oct. 2004. PubMed Central, doi:10.1371/journal.pbio.0020294.
Yang, Wenqi, et al. “Association of Peroxisome Proliferator-Activated Receptor Delta and Additional Gene-Smoking Interaction on Cardiovascular Disease.” Clinical and Experimental Hypertension (New York, N.Y.: 1993), vol. 39, no. 2, 2017, pp. 114–18. PubMed, doi:10.1080/10641963.2016.1210623.
Ye, H. D., et al. “Positive Association between PPARD Rs2016520 Polymorphism and Coronary Heart Disease in a Han Chinese Population.” Genetics and Molecular Research: GMR, vol. 14, no. 2, June 2015, pp. 6350–59. PubMed, doi:10.4238/2015.June.11.10.
Zhou, D., et al. “Vitamin A Deficiency Reduces Liver and Colon Docosahexaenoic Acid Levels in Rats Fed High Linoleic and Low Alpha-Linolenic Acid Diet.” Prostaglandins, Leukotrienes, and Essential Fatty Acids, vol. 71, no. 6, Dec. 2004, pp. 383–89. PubMed, doi:10.1016/j.plefa.2004.07.005.
Zuo, Xiangsheng, et al. “Metastasis Regulation by PPARD Expression in Cancer Cells.” JCI Insight, vol. 2, no. 1, 12 2017, p. e91419. PubMed, doi:10.1172/jci.insight.91419.