Key takeaways:
~ Allergic reactions to antibiotics are fairly common and can be a big problem.
~ Other adverse antibiotic reactions can include delayed reactions or liver damage.
~ Genetic variants can increase susceptibility to antibiotic reactions.
This article is for general informational purposes. Talk to your doctor and pharmacist if you have questions about specific medications.
Antibiotic Reactions: from allergy to liver damage
Imagine being sick, feeling like a truck ran you over… You head to the doctor and receive a prescription for an antibiotic. After dragging yourself through the pharmacy drive-through, you go straight home and take your first dose, expecting relief to soon follow. But low and behold, a little while later you’re covered with an itchy rash and on the phone with your doctor about a possible antibiotic allergy.
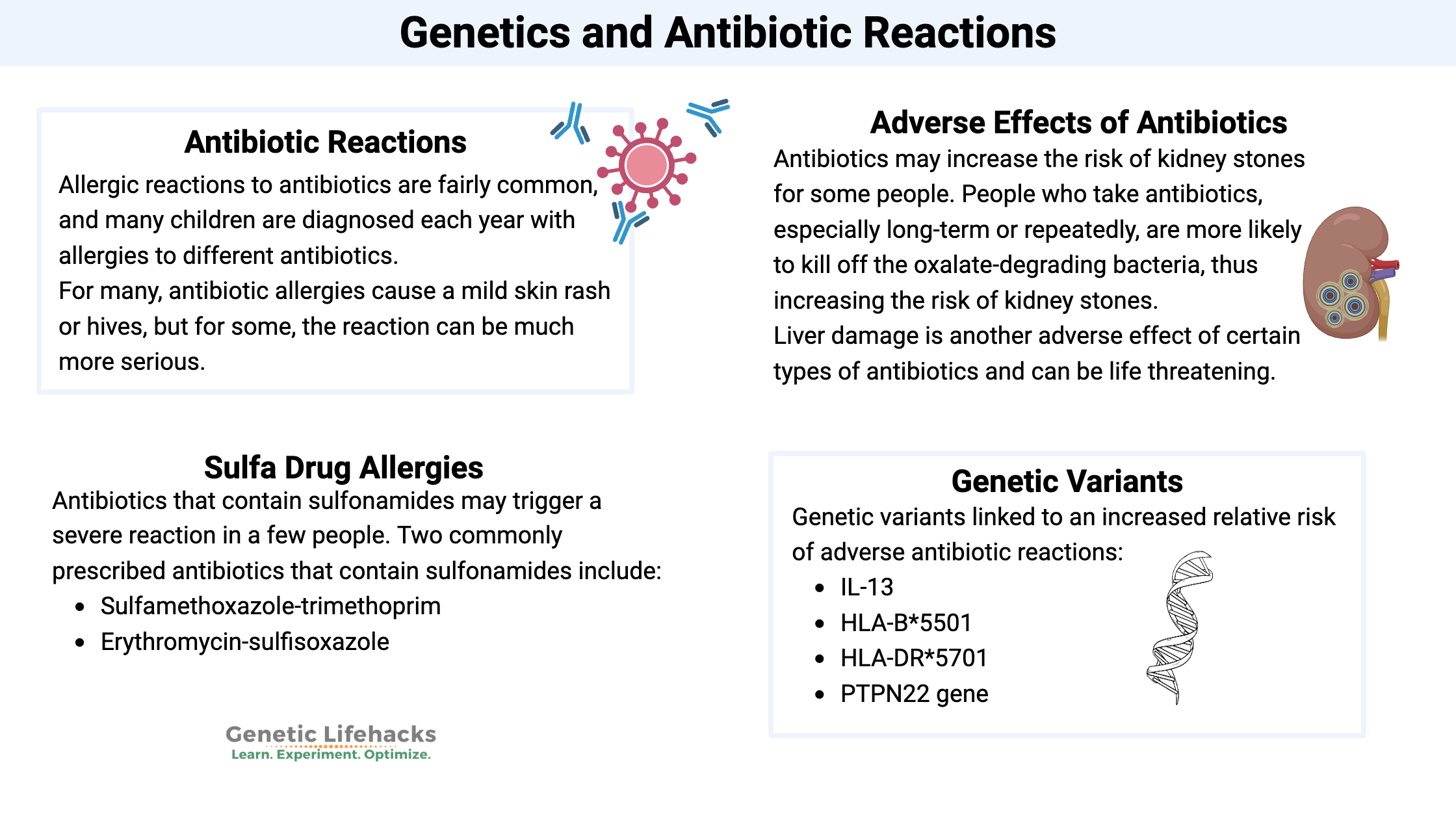
Allergic reactions to antibiotics are fairly common, and many children are diagnosed each year with allergies to different antibiotics.
Adverse drug reactions are more common than you would think. A recent study showed that adverse drug reactions kill more than 100,000 people annually in the US and almost 200,000/per year in Europe.[ref]
One type of adverse drug reaction is an allergic or adverse reaction to antibiotics.
For many, antibiotic allergies cause a mild skin rash or hives, but for some, the reaction can be much more serious or even life-threatening.[ref]
The flip side is that antibiotic allergies are often overdiagnosed. It can happen when a rash occurs, and the cause isn’t totally clear. For example, if a child develops a rash or hives while on an antibiotic, it may be a reaction to the antibiotic or simply due to illness. A diagnosis of possible penicillin (or another antibiotic) allergy goes into the electronic health record.
The problem with overdiagnosis is that either broad-spectrum or inferior antibiotics are then prescribed for that person – often for years or decades. Overuse of broad-spectrum antibiotics can lead to antibiotic-resistant strains. Inferior antibiotics can lead to poor resolution of the illness.[ref]
Sulfa Drug Allergies:
While uncommon, antibiotics that contain sulfonamides may trigger a severe reaction in a few people. Two commonly prescribed antibiotics that contain sulfonamides include:
- Sulfamethoxazole-trimethoprim
- Erythromycin-sulfisoxazole
Reactions to sulfa drugs can be severe. While called a ‘sulfa allergy’, it is technically an IgE reaction that isn’t an allergy, per se, but a potentially life-threatening delayed reaction, often occurring a week or two after starting the antibiotic.[ref]
Penicillin allergies:
Discovered by Alexander Fleming, penicillins have been widely used since the 1940s. Before discovering penicillins, there were no effective treatments for bacterial infections, such as pneumonia, gonorrhea, meningitis, sepsis, and more. While there are modern problems with overuse, antibiotics really are a miracle drug that has saved millions of lives.[ref]
About 10% of the US has a diagnosis of being allergic to penicillin or other β-Lactam antibiotics. β-Lactam antibiotics include penicillins, cephalosporins, carbapenems, and monobactams.[ref]
As I mentioned above, overdiagnosis of penicillin allergy is common.
A skin prick test can confirm the penicillin allergy. Studies show that around 4% of people with a penicillin allergy diagnosis are actually allergic to it.[ref]
One study states: “The overlabeling of pediatric antibiotic allergy represents a huge burden in society. Given that up to 10% of the US population is labeled as penicillin allergic, it can be estimated that at least 5 million children in this country are labeled with penicillin allergy. We now understand that most of the cutaneous symptoms that are interpreted as drug allergy are likely viral induced or due to a drug–virus interaction, and they usually do not represent a long-lasting, drug-specific, adaptive immune response to the antibiotic that a child received. “[ref]
Delayed reactions to antibiotics
Reactions to antibiotics don’t always happen immediately. Sometimes antibiotics can induce a later reaction or trigger longer-term issues.
For example, one study found that an IgE-related gene, MS4A2, was related to the risk of eczema. But that risk substantially increased when combined with antibiotic use in childhood. Eczema is an itchy, red skin rash that is often related to increased IgE antibodies.[ref]
Other adverse effects of antibiotics
Antibiotics may increase the risk of kidney stones for some people. Recent research points to the interaction between Oxalobacter formigenes, the bacteria that degrades oxalates, and kidney stone formation. People who take antibiotics, especially long-term or repeatedly, are more likely to kill off the oxalate-degrading bacteria, thus increasing the risk of kidney stones.[ref]
Liver damage is another adverse effect of certain types of antibiotics. While the liver can usually heal from the damage, it can be life-threatening in some patients.[ref]
Antibiotic Reactions Genotype Report:
Genetic variants combine with other factors in susceptibility to antibiotic reactions.
Please keep in mind that an increased genetic risk does NOT mean that you will automatically be allergic to a drug. Instead, this means that your relative risk of an adverse reaction is higher than if you didn’t carry the variant. Many people with the variants below will never have an adverse reaction to an antibiotic.
Take this information as a ‘heads up‘ to be aware of adverse reactions and seek medical treatment if needed.
The following genetic variants are linked to an increased relative risk of adverse antibiotic reactions.
Lifehacks:
Double-check your antibiotic allergy diagnosis:
Misdiagnosis of penicillin and other antibiotic allergies is a real problem because it limits your options for the best type of antibiotic for certain bacterial infections. For example, using certain antibiotics to avoid penicillin-based drugs may increase your risk of C. difficile infection.[ref] If you were diagnosed with an antibiotic allergy (especially in childhood), you might want to talk with your doctor about getting an allergy test done to confirm it.
Alternatives to antibiotics:
There are many reasons to avoid overusing antibiotics. From a public health perspective, limiting antibiotic use means that we are likely to have fewer antibiotic-resistant bacterial strains emerge. However, it needs to be balanced on an individual basis as to what is best for you.
Before I explain the research on natural options for fighting bacterial infections, I want to be clear that antibiotics are sometimes completely necessary, literally lifesaving. If you are sick with a bacterial infection, talk with your doctor about whether a natural approach could work – and discuss at what point you may need to switch to a prescription antibiotic.
Spices have been used for centuries to flavor food and prevent spoiling. Modern science shows that many of our traditionally used spices are potent natural antimicrobials.
Oregano oil has antimicrobial activity, inhibiting the reproduction of S. aureus, Bacillus subtilis, and E. coli. In fact, oregano essential oil is one of the most effective natural antibiotics for many different bacterial species.[ref]
Rosemary essential oil kills E. coli in a petri dish.[ref][ref] I didn’t find any clinical trials, though, that tested the use in people.
Garlic has been used for centuries as an antimicrobial. Research shows that garlic or garlic extract can inhibit Salmonella, E. coli, Staphylococcus aureus, and other bacteria.
Thyme, cinnamon, clove, ginger, and cumin – traditional spices from different cultures worldwide – all have antimicrobial properties.[ref]
Decreasing urinary tract infections (UTIs) without antibiotics:
Related Articles and Topics:
References:
Adedeji, W. A. “THE TREASURE CALLED ANTIBIOTICS.” Annals of Ibadan Postgraduate Medicine, vol. 14, no. 2, Dec. 2016, p. 56. www.ncbi.nlm.nih.gov, https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC5354621/.
Björnsson, Einar S. “Drug-Induced Liver Injury Due to Antibiotics.” Scandinavian Journal of Gastroenterology, vol. 52, no. 6–7, July 2017, pp. 617–23. PubMed, https://doi.org/10.1080/00365521.2017.1291719.
Blumenthal, Kimberly G., et al. “Antibiotic Allergy.” Lancet (London, England), vol. 393, no. 10167, Jan. 2019, p. 183. www.ncbi.nlm.nih.gov, https://doi.org/10.1016/S0140-6736(18)32218-9.
—. “Antibiotic Allergy.” Lancet (London, England), vol. 393, no. 10167, Jan. 2019, p. 183. www.ncbi.nlm.nih.gov, https://doi.org/10.1016/S0140-6736(18)32218-9.
—. “Antibiotic Allergy.” Lancet (London, England), vol. 393, no. 10167, Jan. 2019, p. 183. www.ncbi.nlm.nih.gov, https://doi.org/10.1016/S0140-6736(18)32218-9.
Cornejo-García, J. A., et al. “A Non-Synonymous Polymorphism in Galectin-3 Lectin Domain Is Associated with Allergic Reactions to Beta-Lactam Antibiotics.” The Pharmacogenomics Journal, vol. 16, no. 1, Feb. 2016, pp. 79–82. PubMed, https://doi.org/10.1038/tpj.2015.24.
Cosby A. Stone, Jr. “The Challenge of De-Labeling Penicillin Allergy.” Allergy, vol. 75, no. 2, Feb. 2020, p. 273. www.ncbi.nlm.nih.gov, https://doi.org/10.1111/all.13848.
Daly, Ann K., et al. “HLA-B*5701 Genotype Is a Major Determinant of Drug-Induced Liver Injury Due to Flucloxacillin.” Nature Genetics, vol. 41, no. 7, July 2009, pp. 816–19. PubMed, https://doi.org/10.1038/ng.379.
—. “HLA-B*5701 Genotype Is a Major Determinant of Drug-Induced Liver Injury Due to Flucloxacillin.” Nature Genetics, vol. 41, no. 7, July 2009, pp. 816–19. PubMed, https://doi.org/10.1038/ng.379.
Gágyor, Ildikó, et al. “Herbal Treatment with Uva Ursi Extract versus Fosfomycin in Women with Uncomplicated Urinary Tract Infection in Primary Care: A Randomized Controlled Trial.” Clinical Microbiology and Infection: The Official Publication of the European Society of Clinical Microbiology and Infectious Diseases, vol. 27, no. 10, Oct. 2021, pp. 1441–47. PubMed, https://doi.org/10.1016/j.cmi.2021.05.032.
Guo, Qin, et al. “Probiotics for the Prevention of Pediatric Antibiotic‐associated Diarrhea.” The Cochrane Database of Systematic Reviews, vol. 2019, no. 4, Apr. 2019. www.ncbi.nlm.nih.gov, https://doi.org/10.1002/14651858.CD004827.pub5.
Hua, Li, et al. “Interaction between Antibiotic Use and MS4A2 Gene Polymorphism on Childhood Eczema: A Prospective Birth Cohort Study.” BMC Pediatrics, vol. 21, no. 1, July 2021, p. 314. BioMed Central, https://doi.org/10.1186/s12887-021-02786-x.
Joshi, Shivam, and David S. Goldfarb. “The Use of Antibiotics and Risk of Kidney Stones.” Current Opinion in Nephrology and Hypertension, vol. 28, no. 4, July 2019, pp. 311–15. PubMed, https://doi.org/10.1097/MNH.0000000000000510.
Krebs, Kristi, et al. “Genome-Wide Study Identifies Association between HLA-B∗55:01 and Self-Reported Penicillin Allergy.” American Journal of Human Genetics, vol. 107, no. 4, Oct. 2020, p. 612. www.ncbi.nlm.nih.gov, https://doi.org/10.1016/j.ajhg.2020.08.008.
—. “Genome-Wide Study Identifies Association between HLA-B∗55:01 and Self-Reported Penicillin Allergy.” American Journal of Human Genetics, vol. 107, no. 4, Oct. 2020, p. 612. www.ncbi.nlm.nih.gov, https://doi.org/10.1016/j.ajhg.2020.08.008.
—. “Genome-Wide Study Identifies Association between HLA-B∗55:01 and Self-Reported Penicillin Allergy.” American Journal of Human Genetics, vol. 107, no. 4, Oct. 2020, p. 612. www.ncbi.nlm.nih.gov, https://doi.org/10.1016/j.ajhg.2020.08.008.
Kullak-Ublick, Gerd A., et al. “Drug-Induced Liver Injury: Recent Advances in Diagnosis and Risk Assessment.” Gut, vol. 66, no. 6, June 2017, p. 1154. www.ncbi.nlm.nih.gov, https://doi.org/10.1136/gutjnl-2016-313369.
Lagha, Rihab, et al. “Antibacterial and Biofilm Inhibitory Activity of Medicinal Plant Essential Oils Against Escherichia Coli Isolated from UTI Patients.” Molecules (Basel, Switzerland), vol. 24, no. 6, Mar. 2019, p. E1161. PubMed, https://doi.org/10.3390/molecules24061161.
Lenger, Stacy M., et al. “D-Mannose vs Other Agents for Recurrent Urinary Tract Infection Prevention in Adult Women: A Systematic Review and Meta-Analysis.” American Journal of Obstetrics and Gynecology, vol. 223, no. 2, Aug. 2020, p. 265.e1. www.ncbi.nlm.nih.gov, https://doi.org/10.1016/j.ajog.2020.05.048.
Liu, Qing, et al. “Antibacterial and Antifungal Activities of Spices.” International Journal of Molecular Sciences, vol. 18, no. 6, June 2017. www.ncbi.nlm.nih.gov, https://doi.org/10.3390/ijms18061283.
—. “Antibacterial and Antifungal Activities of Spices.” International Journal of Molecular Sciences, vol. 18, no. 6, June 2017. www.ncbi.nlm.nih.gov, https://doi.org/10.3390/ijms18061283.
Lucena, M. Isabel, et al. “Susceptibility to Amoxicillin-Clavulanate-Induced Liver Injury Is Influenced by Multiple HLA Class I and II Alleles.” Gastroenterology, vol. 141, no. 1, July 2011, p. 338. www.ncbi.nlm.nih.gov, https://doi.org/10.1053/j.gastro.2011.04.001.
—. “Susceptibility to Amoxicillin-Clavulanate-Induced Liver Injury Is Influenced by Multiple HLA Class I and II Alleles.” Gastroenterology, vol. 141, no. 1, July 2011, p. 338. www.ncbi.nlm.nih.gov, https://doi.org/10.1053/j.gastro.2011.04.001.
Montassier, Emmanuel, et al. “Probiotics Impact the Antibiotic Resistance Gene Reservoir along the Human GI Tract in a Person-Specific and Antibiotic-Dependent Manner.” Nature Microbiology, vol. 6, no. 8, 2021, p. 1043. www.ncbi.nlm.nih.gov, https://doi.org/10.1038/s41564-021-00920-0.
Norton, Allison Eaddy, et al. “Antibiotic Allergy in Pediatrics.” Pediatrics, vol. 141, no. 5, May 2018. www.ncbi.nlm.nih.gov, https://doi.org/10.1542/peds.2017-2497.
Park, Min Jee, et al. “Effect of Early-Life Antibiotic Exposure and IL-13 Polymorphism on Atopic Dermatitis Phenotype.” Pediatric Allergy and Immunology, vol. 32, no. 7, 2021, pp. 1445–54. Wiley Online Library, https://doi.org/10.1111/pai.13531.
Petrolini, Fernanda Villas Boas, et al. “Evaluation of the Antibacterial Potential of Petroselinum Crispum and Rosmarinus Officinalis against Bacteria That Cause Urinary Tract Infections.” Brazilian Journal of Microbiology: [Publication of the Brazilian Society for Microbiology], vol. 44, no. 3, 2013, pp. 829–34. PubMed, https://doi.org/10.1590/S1517-83822013005000061.
“PharmGKB.” PharmGKB, https://www.pharmgkb.org/literature/15101668. Accessed 6 Jan. 2022.
“—.” PharmGKB, https://www.pharmgkb.org/literature/15101668. Accessed 6 Jan. 2022.
Schnyder, Benno, and Werner J. Pichler. “Allergy to Sulfonamides.” Journal of Allergy and Clinical Immunology, vol. 131, no. 1, Jan. 2013, pp. 256-257.e5. www.jacionline.org, https://doi.org/10.1016/j.jaci.2012.10.003.
Serpa, Jose A., et al. “Prevalence of G6PD Deficiency in a Large Cohort of HIV-Infected Patients.” The Journal of Infection, vol. 61, no. 5, Nov. 2010, pp. 399–402. PubMed, https://doi.org/10.1016/j.jinf.2010.08.003.
Tohkin, M., et al. “A Whole-Genome Association Study of Major Determinants for Allopurinol-Related Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis in Japanese Patients.” The Pharmacogenomics Journal, vol. 13, no. 1, Feb. 2013, pp. 60–69. PubMed, https://doi.org/10.1038/tpj.2011.41.
Trubiano, Jason A., et al. “The Three C’s of Antibiotic Allergy – Classification, Cross-Reactivity and Collaboration.” The Journal of Allergy and Clinical Immunology. In Practice, vol. 5, no. 6, Dec. 2017, p. 1532. www.ncbi.nlm.nih.gov, https://doi.org/10.1016/j.jaip.2017.06.017.
Wolkenstein, P., et al. “Prospective Evaluation of Detoxification Pathways as Markers of Cutaneous Adverse Reactions to Sulphonamides in AIDS.” Pharmacogenetics, vol. 10, no. 9, Dec. 2000, pp. 821–28. PubMed, https://doi.org/10.1097/00008571-200012000-00007.
Yang, Y., et al. “HLA-B*51:01 Is Strongly Associated with Clindamycin-Related Cutaneous Adverse Drug Reactions.” The Pharmacogenomics Journal, vol. 17, no. 6, Dec. 2017, pp. 501–05. PubMed, https://doi.org/10.1038/tpj.2016.61.
..