It may be odd to think of a ‘sleep supplement’ as possibly helping to prevent or treat COVID-19…But the research on melatonin over the past couple of decades shows that it plays an important role in our body’s inflammatory response to pathogens.
This article covers the current research on melatonin for COVID-19 and explains the science behind how it impacts immune response. As always, talk with your doctor if you have any questions on whether a supplement is right for you.
Related article: Research roundup: Preventing and Mitigating Covid-19
Melatonin, SARS-CoV-2, and Immune System Response
Melatonin is a hormone released in larger amounts at night. It is produced in the pineal gland.
 The pineal gland, a little organ nestled in the center of the brain, cranks up the production of melatonin in response to darkness.
The pineal gland, a little organ nestled in the center of the brain, cranks up the production of melatonin in response to darkness.
While we often think of melatonin as a ‘sleep hormone’, it really is more of a circadian rhythm setting hormone. Research on melatonin shows that it doesn’t work to make you sleepy, like a sleeping pill, but it tells your body that it is night.[ref]
Fun fact: Melatonin is produced by all living organisms, from bacteria to plants to humans.[ref]
Melatonin, though, is way more than just a sleep hormone…
What does melatonin do in the body?
The majority of the melatonin in the body is produced at night in the pineal gland and then circulated throughout the body. On a cellular level, though, most cells can synthesize small amounts of melatonin, acting within the cell in a bunch of nifty ways.
Antioxidant: Within cells, melatonin is produced at low levels throughout the day and night. It acts as an intracellular antioxidant, protecting cells from oxidative stress.[ref]
Cancer prevention: Through its role in neutralizing oxidation, melatonin protects cells against the DNA damage that causes cancer. Additionally, in cancer, melatonin has anticancer actions and is being used along with chemotherapy.[ref]
Blood pressure: Melatonin is involved in blood pressure regulation and the pattern of blood pressure dipping down at night. Clinical trials show that regularly taking timed-release melatonin at night reduces blood pressure. (Note that fast-release melatonin is ineffective here)[ref][ref][ref]
Immune system: In addition to its role in circadian rhythm and immune response, melatonin acts directly to boost the immune system’s initial response to a virus or bacteria. Melatonin also prevents an excessive response – such as in ARDS or sepsis.[ref]
Reduction of melatonin in aging:
The pineal gland begins to calcify as we get older. The calcification reduces the amount of melatonin the pineal gland can produce.
Here is a chart showing the peak in melatonin production around puberty and the downhill path in aging.
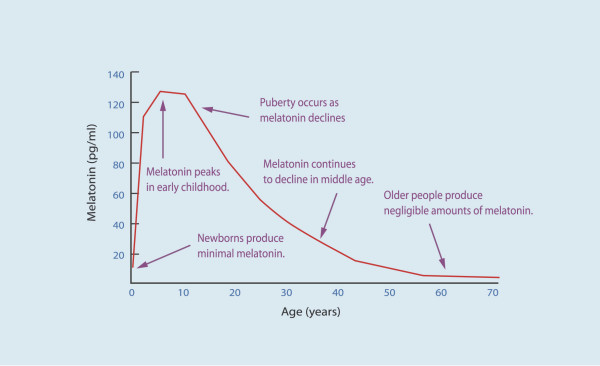
The significant decrease in melatonin with aging is thought to be one of the reasons for neurodegenerative diseases, such as Alzheimer’s. Additionally, the melatonin decrease adds to reduced immune response and increased cancer risk in aging.[ref]
Melatonin and the immune response:
Melatonin does a lot in the immune system.
In a nutshell, it modulates immune response – boosting the needed initial response and tamping down excessive proinflammatory cytokines. Balance.[ref][ref]
Animal studies over the last few decades show that melatonin regulates immune response. For example, research shows that melatonin is an effective treatment for pathogenic infections when given either before or during the infection.[ref] Extra melatonin is helpful in mice who are fighting off Staph or E. coli infections – especially during a ‘short photoperiod’ which mimics winter sunlight.[ref]
In human clinical trials, melatonin helps to reduce H. pylori infections.[ref] Other studies show that melatonin may help fight off various bacterial pathogens, including tuberculosis, staph, and MRSA.[ref] Melatonin may also be important in protecting against sepsis and septic shock.[ref]
Studies on viruses show that melatonin is beneficial in fighting off a variety of viruses including:[ref]
In some cases, supplemental melatonin is preventing an overactivation of the host immune response, and in other cases, melatonin is boosting the body’s initial immune response.[ref]
“Viruses induce an explosion of inflammatory cytokines and reactive oxygen species, and melatonin is the best natural antioxidant that is lost with age.”[ref]
Clinical Trials of Melatonin as a Treatment for covid-19
Many research papers have been written on melatonin for the prevention of COVID-19 and as a treatment for COVID-19.
Theoretically, melatonin inhibits COVID-19:
Many research articles discuss the theory of why melatonin would be an ideal supplement to take for preventing and treating SAR-CoV-2 infections. I’ll let you read through them for yourself if you want to learn more about the mechanism of action for melatonin in viral infections.[ref][ref][ref][ref][ref]
Computer-predicted drug repurposing studies: The first study to catch my eye – way back at the very start of the pandemic in March 2020 – predicted which currently available drugs could be useful in fighting off the SARS-CoV-2 virus. Melatonin was one of the drugs that the computer model showed would target what at that time was dubbed “2019 novel coronavirus”.[ref]
Another in silco study shows that melatonin may directly block SARS-CoV-2 replication, in conjunction with another medication, pirfenidone.[ref]
Reduced risk of getting COVID:
Using supplemental melatonin at night reduces the likelihood of testing positive for COVID-19 by 28%. The study looked at medical information on more than 26,000 people to make the connection between taking melatonin at night and reduced risk of a positive lab test for SARS-CoV-2.[ref]
Melatonin for COVID patients: Treating the cytokine storm
An NIH-sponsored study of melatonin given to intubated COVID-19 patients showed that it significantly reduced mortality rates. The study used hospital records of about 1,000 severe COVID-19 patients.[ref]
A small randomized clinical trial in Iran of 3mg melatonin three times a day for hospitalized moderate COVID patients showed decreases in symptoms and shorter hospital stay.[ref]
In contrast, IV melatonin, zinc, and vitamin C showed that there was no significant effect on ICU length of stay in a small Iranian trial.[ref]
A 2022 placebo-controlled trial found that melatonin was effective in treating severe COVID-19.[ref]
An Iraqi clinical trial in hospitalized COVID-19 patients found that melatonin cut the risk of thrombosis by 50%, sepsis by more than 50%, and cut the risk of death by more than 90%. Of the 184 patients in the trial, one patient in the melatonin group died compared to 13 in the control group. The hospital gave the patients Natrol 10mg melatonin pills each night about a half hour before they went to sleep. [ref]
A 2024 placebo-controlled trial found that melatonin, along with a mixture of vitamins including zinc, was effective in treating the symptoms of COVID-19 and “accelerating its disappearance” when taken daily. [ref]
Dose and timing of supplemental melatonin:
I can’t give you a “take X amount” recommendation because everyone is different.
Things to consider:
Supplemental melatonin is taken before bedtime. If you are wanting to shift your bedtime forward, one way to make this shift is to take melatonin earlier each night. This can be really helpful if you are going to be traveling east across several time zones.
The ‘dose’ for melatonin likely depends a lot on your age and whether you are using electronic devices at night. Blue light from your TV, cell phone, iPad, etc can suppress melatonin levels quite a bit. If you regularly are on your phone for hours before bed, then you may need more melatonin.
Older people have decreased melatonin production (see the graph above) compared to youngsters. Thus, if you are older, you likely need a higher dose of melatonin at night than someone younger.
Standard melatonin pills initially give a big boost in melatonin, but melatonin’s half-life is fairly short (around 45 minutes).[ref]
Here is a graph of how quickly melatonin is metabolized:[CC license ref]
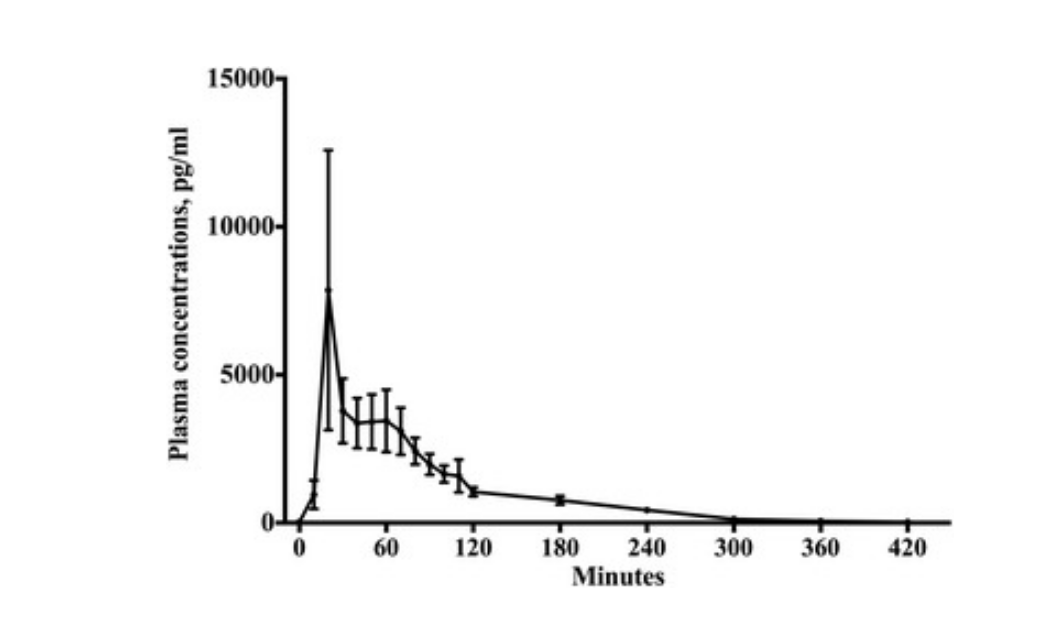
Timed-release melatonin better mimics what the pineal gland produces at night. Timed-release, also marketed as sustained-release, melatonin spreads out the release over six hours or so.
For timed-release melatonin, you can get it in doses of 300 mcg (.3 mg) up through 10 mg on Amazon or at health food stores. It’s fairly inexpensive – often around $3 for a month’s supply.
If you aren’t used to taking melatonin, you may want to start with a lower dose. You can always double it after a few weeks.
The recent clinical trial on melatonin in hospitalized COVID patients (Iraq) used a dose of 10 mg/night while the patients were in the hospital.
Related article: Supplemental Melatonin
Personal anecdote time:
When I tried melatonin when I was in my 30’s, it made me feel kind of groggy and headachy the next morning. I don’t remember the dose, just that I didn’t like it. Decided that I would never take it again.
A few years ago, I decided that the research studies on melatonin for preventing Alzheimer’s were impressive, but I remembered not liking melatonin. I started with the 300 mcg (0.3 mg) timed-release melatonin and then doubled it after a month or so. Next, I moved up to 1 mg of timed release, and now, a few years in, I take 3 mg of timed-release melatonin most nights (when I remember it).
Everyone is unique. The point of my personal experience is that you don’t have to start with a high dose – and you can change it up as you go. Often, I’ve read about a supplement and thought that I needed to take an exact dose all the time. But that isn’t true – for melatonin and many other supplements. Go with what fits your situation.
Genetics and melatonin production:
Tryptophan is an essential amino acid that we get from foods that contain protein. It is the precursor for serotonin and melatonin.
Essentially, tryptophan can take two pathways in the body:
- it can go down the kynurenine pathway and eventually make niacin, especially in niacin deficiency
- it can be used to make serotonin, which then can be methylated to become melatonin
Both paths are important, but you want balance there. Kynurenine can become a neurotoxic substance called quinolinic acid, which you want to avoid.
A couple of genetic variants in the tryptophan hydroxylase (TPH2) shift a person towards naturally producing a little less serotonin/melatonin.
Members: Log in and select your data file
Not a member? Join now to see your data below.
TPH2 gene: codes for the enzyme that converts tryptophan to 5-HTP, which then gets converted to serotonin in the brain.
Check your genetic data for rs4570625 (23andMe v4, v5; AncestryDNA):
- G/G: typical, less tryptophan conversion to serotonin/melatonin[ref] a higher risk of depression, suicidal depression[ref][ref]
- G/T: somewhat decreased risk of depression
- T/T: more conversion to serotonin, generally decreased risk of depression[ref], less aggressiveness, and lower anxiety[ref]
Members: Your genotype for rs4570625 is —.
Check your genetic data for rs11178997 (23andMe v4; AncestryDNA):
- T/T: typical
- A/T: less tryptophan conversion to serotonin, somewhat increased risk of depression
- A/A: less tryptophan conversion to serotonin/melatonin, increased risk of depression and suicide[ref][ref]
Members: Your genotype for rs11178997 is —.
Conclusion:
There is a lot of junk ‘science’ making the rounds when it comes to COVID-19. For example, a really popular naturopath on Facebook is promoting eating kimchi to make covid ‘antibody’. Hmm…
I encourage all of you to check the research sources – including for this article – and make informed decisions.
My personal criteria when looking at a supplement is to weigh the benefits vs. risks. The safety record is strong and there is little risk in taking melatonin. The benefits, especially in someone middle-aged or older, are well documented and fairly substantial.
The research studies so far on melatonin for COVID-19 show some promise, but the results of large, randomized double-blind placebo-controlled trials are not yet available. (A couple of clinical trials were registered last year, but no results are posted.)
Without the ‘gold standard’ of evidence, I personally look at the risk vs. possible benefits. For me, the possible benefits are big and the risk is very small. Plus, my cynical side says that there is no money in promoting melatonin for COVID-19 prevention, and thus, it is unlikely that a lot of clinical trials will be done here.
Again – I encourage everyone to read through the research and make their own decisions. Melatonin is just one ‘tool’ to have in the toolbox for preventing illnesses.
Related Articles and Genes:
Tryptophan: Building block for serotonin and melatonin
Tryptophan metabolism influences mood, sleep, neurotransmitters, and immune response.
Melatonin: Key to Health and Longevity
It seems like everything that I’ve written about lately has a common thread: melatonin. When I started weaving together all those melatonin threads, a big picture was revealed. You could say it is a… tapestry of health.
COVID-19 & Genetics: Who gets sick and why?
Genetic variants play a role in susceptibility to infectious diseases. Not everyone will get the norovirus or a particular strain of the flu — due to genetic variants. New research shows that genetics also plays a role in the severity of COVID-19.
References:
Andersen, L. P. H., Werner, M. U., Rosenkilde, M. M., Harpsøe, N. G., Fuglsang, H., Rosenberg, J., & Gögenur, I. (2016b). Pharmacokinetics of oral and intravenous melatonin in healthy volunteers. BMC Pharmacology & Toxicology, 17, 8. https://doi.org/10.1186/s40360-016-0052-2
Anderson, G., Maes, M., Markus, R. P., & Rodriguez, M. (2015). Ebola virus: Melatonin as a readily available treatment option. Journal of Medical Virology, 87(4), 537–543. https://doi.org/10.1002/jmv.24130
Anderson, G., & Reiter, R. J. (2020). Melatonin: Roles in influenza, Covid‐19, and other viral infections. Reviews in Medical Virology, 30(3), e2109. https://doi.org/10.1002/rmv.2109
Artigas, L., Coma, M., Matos-Filipe, P., Aguirre-Plans, J., Farrés, J., Valls, R., Fernandez-Fuentes, N., Haba-Rodriguez, J. de la, Olvera, A., Barbera, J., Morales, R., Oliva, B., & Mas, J. M. (2020). In-silico drug repurposing study predicts the combination of pirfenidone and melatonin as a promising candidate therapy to reduce SARS-CoV-2 infection progression and respiratory distress caused by cytokine storm. PLOS ONE, 15(10), e0240149. https://doi.org/10.1371/journal.pone.0240149
Baehne, C. G., Ehlis, A.-C., Plichta, M. M., Conzelmann, A., Pauli, P., Jacob, C., Gutknecht, L., Lesch, K.-P., & Fallgatter, A. J. (2009). Tph2 gene variants modulate response control processes in adult ADHD patients and healthy individuals. Molecular Psychiatry, 14(11), 1032–1039. https://doi.org/10.1038/mp.2008.39
Bahrampour Juybari, K., Pourhanifeh, M. H., Hosseinzadeh, A., Hemati, K., & Mehrzadi, S. (2020). Melatonin potentials against viral infections including COVID-19: Current evidence and new findings. Virus Research, 287, 198108. https://doi.org/10.1016/j.virusres.2020.198108
Bhattacharya, S., Patel, K. K., Dehari, D., Agrawal, A. K., & Singh, S. (2019). Melatonin and its ubiquitous anticancer effects. Molecular and Cellular Biochemistry, 462(1–2), 133–155. https://doi.org/10.1007/s11010-019-03617-5
Bishayi, B., Adhikary, R., Nandi, A., & Sultana, S. (2016). Beneficial effects of exogenous melatonin in acute staphylococcus aureus and escherichia coli infection-induced inflammation and associated behavioral response in mice after exposure to short photoperiod. Inflammation, 39(6), 2072–2093. https://doi.org/10.1007/s10753-016-0445-9
Boga, J. A., Coto‐Montes, A., Rosales‐Corral, S. A., Tan, D., & Reiter, R. J. (2012). Beneficial actions of melatonin in the management of viral infections: A new use for this “molecular handyman”? Reviews in Medical Virology, 22(5), 323–338. https://doi.org/10.1002/rmv.1714
Bonilla, E., Valero, N., Chacín-Bonilla, L., Pons, H., Larreal, Y., Medina-Leendertz, S., & Espina, L. M. (2003a). Melatonin increases interleukin-1beta and decreases tumor necrosis factor alpha in the brain of mice infected with the Venezuelan equine encephalomyelitis virus. Neurochemical Research, 28(5), 681–686. https://doi.org/10.1023/a:1022897314108
Bonilla, E., Valero, N., Chacín-Bonilla, L., Pons, H., Larreal, Y., Medina-Leendertz, S., & Espina, L. M. (2003b). Melatonin increases interleukin-1beta and decreases tumor necrosis factor alpha in the brain of mice infected with the Venezuelan equine encephalomyelitis virus. Neurochemical Research, 28(5), 681–686. https://doi.org/10.1023/a:1022897314108
Celinski, K., Konturek, P. C., Konturek, S. J., Slomka, M., Cichoz-Lach, H., Brzozowski, T., & Bielanski, W. (2011). Effects of melatonin and tryptophan on healing of gastric and duodenal ulcers with Helicobacter pylori infection in humans. Journal of Physiology and Pharmacology: An Official Journal of the Polish Physiological Society, 62(5), 521–526.
Claustrat, B., & Leston, J. (2015). Melatonin: Physiological effects in humans. Neuro-Chirurgie, 61(2–3), 77–84. https://doi.org/10.1016/j.neuchi.2015.03.002
Cross, K. M., Landis, D. M., Sehgal, L., & Payne, J. D. (2021). Melatonin for the early treatment of covid-19: A narrative review of current evidence and possible efficacy. Endocrine Practice, 27(8), 850–855. https://doi.org/10.1016/j.eprac.2021.06.001
Darban, M., Malek, F., Memarian, M., Gohari, A., Kiani, A., Emadi, A., Lavvaf, S., & Bagheri, B. (2021). Efficacy of high dose vitamin c, melatonin and zinc in iranian patients with acute respiratory syndrome due to coronavirus infection: A pilot randomized trial. Journal of Cellular & Molecular Anesthesia, 6(2), 164–167. https://doi.org/10.22037/jcma.v6i2.32182
Efficacy of a low dose of melatonin as an adjunctive therapy in hospitalized patients with covid-19: A randomized, double-blind clinical trial. (2021). Archives of Medical Research. https://doi.org/10.1016/j.arcmed.2021.06.006
El-Missiry, M. A., El-Missiry, Z. M. A., & Othman, A. I. (2020). Melatonin is a potential adjuvant to improve clinical outcomes in individuals with obesity and diabetes with coexistence of Covid-19. European Journal of Pharmacology, 882, 173329. https://doi.org/10.1016/j.ejphar.2020.173329
Gao, J., Pan, Z., Jiao, Z., Li, F., Zhao, G., Wei, Q., Pan, F., & Evangelou, E. (2012). Tph2 gene polymorphisms and major depression – a meta-analysis. PLoS ONE, 7(5), e36721. https://doi.org/10.1371/journal.pone.0036721
Grivas, T. B., & Savvidou, O. D. (2007). Melatonin the “light of night” in human biology and adolescent idiopathic scoliosis. Scoliosis, 2(1), 6. https://doi.org/10.1186/1748-7161-2-6
Grossman, E., Laudon, M., & Zisapel, N. (2011). Effect of melatonin on nocturnal blood pressure: Meta-analysis of randomized controlled trials. Vascular Health and Risk Management, 7, 577–584. https://doi.org/10.2147/VHRM.S24603
Hadi, A., Ghaedi, E., Moradi, S., Pourmasoumi, M., Ghavami, A., & Kafeshani, M. (2019). Effects of melatonin supplementation on blood pressure: A systematic review and meta-analysis of randomized controlled trials. Hormone and Metabolic Research = Hormon- Und Stoffwechselforschung = Hormones Et Metabolisme, 51(3), 157–164. https://doi.org/10.1055/a-0841-6638
Hardeland, R. (2019). Aging, melatonin, and the pro- and anti-inflammatory networks. International Journal of Molecular Sciences, 20(5), 1223. https://doi.org/10.3390/ijms20051223
He, F., Wu, X., Zhang, Q., Li, Y., Ye, Y., Li, P., Chen, S., Peng, Y., Hardeland, R., & Xia, Y. (2021). Bacteriostatic potential of melatonin: Therapeutic standing and mechanistic insights. Frontiers in Immunology, 12, 683879. https://doi.org/10.3389/fimmu.2021.683879
Hu, W., Deng, C., Ma, Z., Wang, D., Fan, C., Li, T., Di, S., Gong, B., Reiter, R. J., & Yang, Y. (2017a). Utilizing melatonin to combat bacterial infections and septic injury. British Journal of Pharmacology, 174(9), 754–768. https://doi.org/10.1111/bph.13751
Hu, W., Deng, C., Ma, Z., Wang, D., Fan, C., Li, T., Di, S., Gong, B., Reiter, R. J., & Yang, Y. (2017b). Utilizing melatonin to combat bacterial infections and septic injury. British Journal of Pharmacology, 174(9), 754–768. https://doi.org/10.1111/bph.13751
Huang, S.-H., Cao, X.-J., Liu, W., Shi, X.-Y., & Wei, W. (2010). Inhibitory effect of melatonin on lung oxidative stress induced by respiratory syncytial virus infection in mice. Journal of Pineal Research, 48(2), 109–116. https://doi.org/10.1111/j.1600-079X.2009.00733.x
Laas, K., Kiive, E., Mäestu, J., Vaht, M., Veidebaum, T., & Harro, J. (2017). Nice guys: Homozygocity for the TPH2 -703G/T (Rs4570625) minor allele promotes low aggressiveness and low anxiety. Journal of Affective Disorders, 215, 230–236. https://doi.org/10.1016/j.jad.2017.03.045
Martín Giménez, V. M., Inserra, F., Tajer, C. D., Mariani, J., Ferder, L., Reiter, R. J., & Manucha, W. (2020). Lungs as target of COVID-19 infection: Protective common molecular mechanisms of vitamin D and melatonin as a new potential synergistic treatment. Life Sciences, 254, 117808. https://doi.org/10.1016/j.lfs.2020.117808
Ramlall, V., Zucker, J., & Tatonetti, N. (2020). Melatonin is significantly associated with survival of intubated COVID-19 patients. MedRxiv, 2020.10.15.20213546. https://doi.org/10.1101/2020.10.15.20213546
Reiter, R. J., Mayo, J. C., Tan, D.-X., Sainz, R. M., Alatorre-Jimenez, M., & Qin, L. (2016). Melatonin as an antioxidant: Under promises but over delivers. Journal of Pineal Research, 61(3), 253–278. https://doi.org/10.1111/jpi.12360
Reiter, R. J., Tan, D.-X., Zhou, Z., Cruz, M. H. C., Fuentes-Broto, L., & Galano, A. (2015). Phytomelatonin: Assisting plants to survive and thrive. Molecules, 20(4), 7396–7437. https://doi.org/10.3390/molecules20047396
Scheer, F. A. J. L., Van Montfrans, G. A., van Someren, E. J. W., Mairuhu, G., & Buijs, R. M. (2004). Daily nighttime melatonin reduces blood pressure in male patients with essential hypertension. Hypertension (Dallas, Tex.: 1979), 43(2), 192–197. https://doi.org/10.1161/01.HYP.0000113293.15186.3b
Shneider, A., Kudriavtsev, A., & Vakhrusheva, A. (2020a). Can melatonin reduce the severity of COVID-19 pandemic? International Reviews of Immunology, 39(4), 153–162. https://doi.org/10.1080/08830185.2020.1756284
Shneider, A., Kudriavtsev, A., & Vakhrusheva, A. (2020b). Can melatonin reduce the severity of COVID-19 pandemic? International Reviews of Immunology, 39(4), 153–162. https://doi.org/10.1080/08830185.2020.1756284
Tan, D. X., Xu, B., Zhou, X., & Reiter, R. J. (2018). Pineal calcification, melatonin production, aging, associated health consequences and rejuvenation of the pineal gland. Molecules : A Journal of Synthetic Chemistry and Natural Product Chemistry, 23(2), 301. https://doi.org/10.3390/molecules23020301
TPH2 -703G/T SNP may have important effect on susceptibility to suicidal behavior in major depression. (2009). Progress in Neuro-Psychopharmacology and Biological Psychiatry, 33(3), 403–409. https://doi.org/10.1016/j.pnpbp.2008.12.013
TPH2 polymorphisms across the spectrum of psychiatric morbidity: A systematic review and meta-analysis. (2018a). Neuroscience & Biobehavioral Reviews, 92, 29–42. https://doi.org/10.1016/j.neubiorev.2018.05.018
TPH2 polymorphisms across the spectrum of psychiatric morbidity: A systematic review and meta-analysis. (2018b). Neuroscience & Biobehavioral Reviews, 92, 29–42. https://doi.org/10.1016/j.neubiorev.2018.05.018
Yang, J., Zhao, X., Ma, J., Qiao, Z., Yang, X., Zhao, E., Ban, B., Zhu, X., Cao, D., Yang, Y., & Qiu, X. (2019). The interaction of tph2 and 5-ht2a polymorphisms on major depressive disorder susceptibility in a chinese han population: A case-control study. Frontiers in Psychiatry, 10, 172. https://doi.org/10.3389/fpsyt.2019.00172
Zhou, Y., Hou, Y., Shen, J., Huang, Y., Martin, W., & Cheng, F. (2020). Network-based drug repurposing for novel coronavirus 2019-nCoV/SARS-CoV-2. Cell Discovery, 6(1), 1–18. https://doi.org/10.1038/s41421-020-0153-3
Zhou, Y., Hou, Y., Shen, J., Mehra, R., Kallianpur, A., Culver, D. A., Gack, M. U., Farha, S., Zein, J., Comhair, S., Fiocchi, C., Stappenbeck, T., Chan, T., Eng, C., Jung, J. U., Jehi, L., Erzurum, S., & Cheng, F. (2020). A network medicine approach to investigation and population-based validation of disease manifestations and drug repurposing for COVID-19. PLOS Biology, 18(11), e3000970. https://doi.org/10.1371/journal.pbio.3000970