Key takeaways:
~Rheumatoid arthritis (RA) is a form of joint pain that is caused by an autoimmune attack. About 1% of the population deals with the pain of RA.
~Genetic variants increase the risk of rheumatoid arthritis, and understanding which genes are involved may help you find individualized solutions.
This article explains what causes RA, the different genes that increase susceptibility to RA, and possible solutions based on the genetic variants.
Members will see their genotype report below and the solutions in the Lifehacks section. Consider joining today.What causes rheumatoid arthritis?
Rheumatoid arthritis is caused by an immune system attack on the joints, causing thickening and inflammation of the joint capsule.[ref]
While RA mainly attacks the joints in the fingers and toes, it can also cause problems with the larger joints and inflammation in organs such as the eyes, lungs, and blood vessels. RA can come and go in ‘attacks’.[ref]
Synovial joint inflammation:
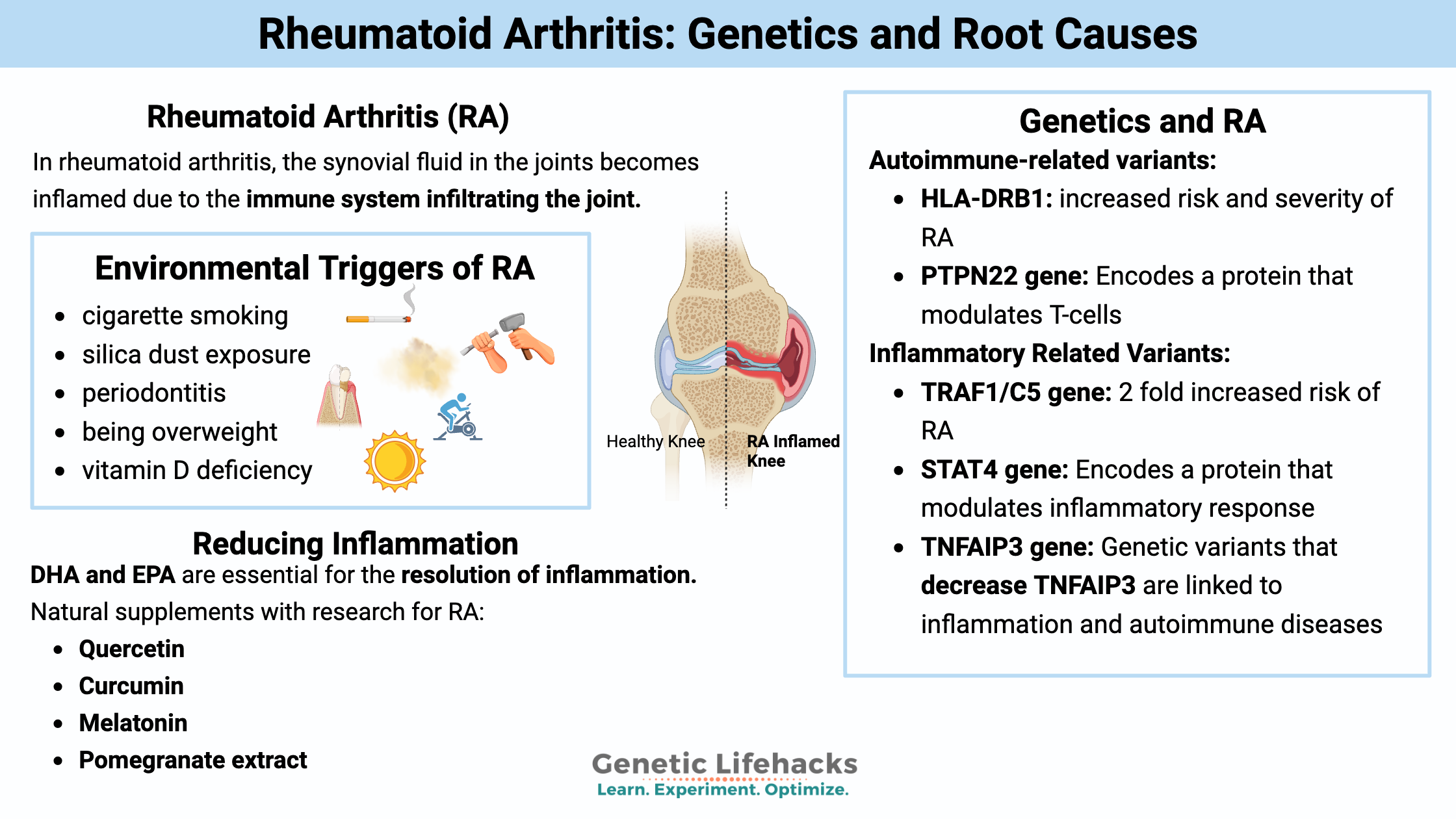
In rheumatoid arthritis, the synovial fluid in the joints becomes inflamed due to the immune system infiltrating the joint. Autoantibodies, including RF (rheumatoid factor) and ACPA (anti-citrullinated protein antibodies), are thought to form immune complexes in the joint that trigger other immune cells to be activated, ratcheting up the inflammation.[ref]
Environmental risk factors:
Risk factors or potential environmental triggers for RA include:[ref]
- cigarette smoking
- silica dust exposure[ref]
- periodontitis (and oral microbiome)[ref]
- being overweight (increases the relative risk by about 5%)
- vitamin D deficiency
One recent study found that an environmental trigger for RA for military veterans was exposure to military waste disposal or burn pits. Both of those exposures caused a 5-fold increase in the risk for anti-CCP antibodies and RA.[ref]
Is rheumatoid arthritis genetic?
Rheumatoid arthritis is thought to develop due to a combination of environmental triggers and genetic susceptibility. Not everyone with genetic susceptibility will get RA. Likewise, not everyone exposed to the same environmental factors will end up with RA.
The heritability of RA is estimated to be ~60%. Heritability is a scientific term that refers to the inherited portion of the risk factors. Thus, RA is both genetic and due to other environmental and autoimmune factors.[ref]
Anticitrullinated Protein Antibodies
Let’s go a little more in-depth on the antibodies and how this ties into the environmental risk factors, such as gingivitis.
One test for RA looks at anticitrullinated protein antibodies (ACPA), which are found in between 55-91% of people with RA. The presence of ACPA alone can’t determine RA, though. A large study that looked at 40,000+ participants showed that 1% of people had elevated ACPA levels. Of those with high ACPA levels, about 22% had RA. [ref]
RA can be broken into two types: ACPA negative and ACPA positive.
Recent research shows that the oral bacteria, Porphyromonas gingivalis, is linked to ACPA production. This bacteria cross-reacts with other bacteria and fungi (such as Candida and Aspergillus) as well as plants (rice, tomatoes, and soy) in producing the ACPA response.[ref]
From one study: “Our findings demonstrate, for the first time, that a monoclonal ACPA (CCP-Ab1) derived from RA patients cross-reacts not only with various autoantigens but also with numerous plant and microbial proteins. We propose that countless environmental factors, including microbes and diet, may trigger the generation of ACPAs that then cross-react with various citrullinated human autoantigens through molecular mimicry to induce RA.“[ref]
Recently, another study pointed toward another microbial cause.
The researchers found that a type of gut microbe, in the genus Subdoligranulum, may be the culprit. These microbes bind to RA monoclonal antibodies, activate T cells, and induce serum RA–relevant IgG autoantibodies. The researchers believe that intestinal mucosa and resident gut bacteria are a driving factor in RA.[ref]
Overgrowth of nerves?
New research shows that for some people who are resistant to the RA drugs that suppress the immune response, the problem instead could be an overgrowth of nerves. The researchers identified genes that were overexpressed in the joints of patients with RA and found that they were associated with increased nerve growth. [ref]
Rheumatoid Arthritis Genotype Report:
Access this content:
An active subscription is required to access this content.
Related Articles and Topics:
Mast Cells: MCAS, Genetics, and Solutions
Mast cells are an important part of your innate immune system. They are front-line defenders against pathogens and allergens. For some people, mast cells can be triggered too easily, giving allergy-like responses to lots of different substances.
TNF-Alpha: Higher innate levels of this inflammatory cytokine
Do you feel like you are always dealing with inflammation? Joint pain, food sensitivity, etc? Perhaps you are genetically geared towards a higher inflammatory response. Tumor necrosis factor (TNF) is an inflammatory cytokine that acts as a signaling molecule in our immune system.
HLA-B27: Increased risk of autoimmune diseases
Our immune system does an awesome job (most of the time) of fighting off pathogenic bacteria and viruses. But to fight off these pathogens, the body needs to know that they are the bad guys. This is where the HLA system comes in.
Debbie Moon is a biologist, engineer, author, and the founder of Genetic Lifehacks where she has helped thousands of members understand how to apply genetics to their diet, lifestyle, and health decisions. With more than 10 years of experience translating complex genetic research into practical health strategies, Debbie holds a BS in engineering from Colorado School of Mines and an MSc in biological sciences from Clemson University. She combines an engineering mindset with a biological systems approach to explain how genetic differences impact your optimal health.