At the top of my supplement list is melatonin, and it has nothing to do with how well I sleep! Instead, the benefits of this ‘sleep hormone’ are many and varied, including boosting immune function, preventing Alzheimer’s disease, and staving off osteoporosis.
This article explains how your body makes melatonin, the decrease in production with aging, the latest research studies on supplemental melatonin, and genetic variants that impact how melatonin works for you. Stick with me, it’s a long one…
Melatonin: More than just a sleep hormone
Melatonin is a hormone synthesized by the pineal gland at night. The pineal gland releases it, and it circulates throughout the body. As a hormone, melatonin has various functions, including synchronizing the day-night cycle.
How is melatonin created?
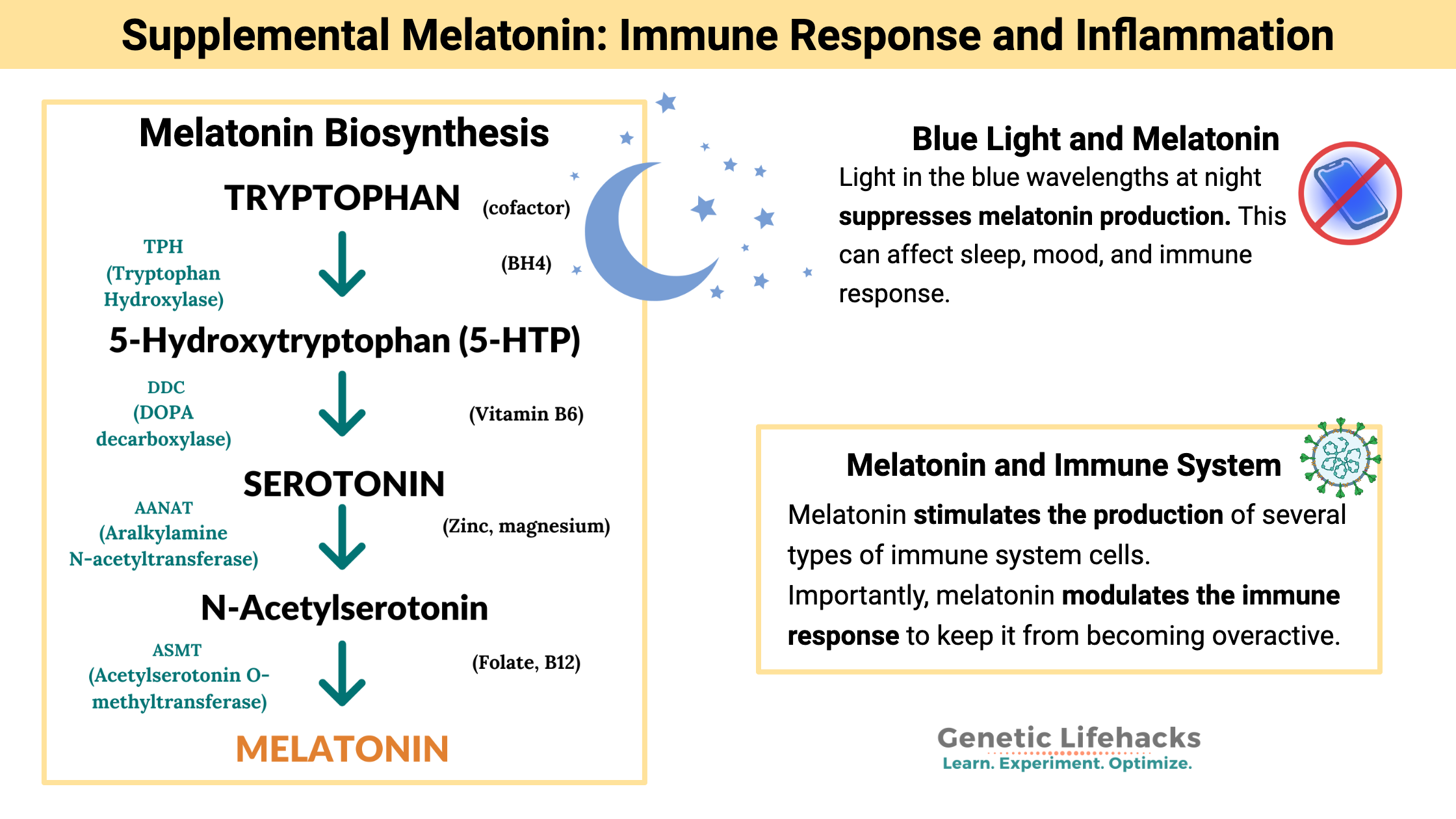
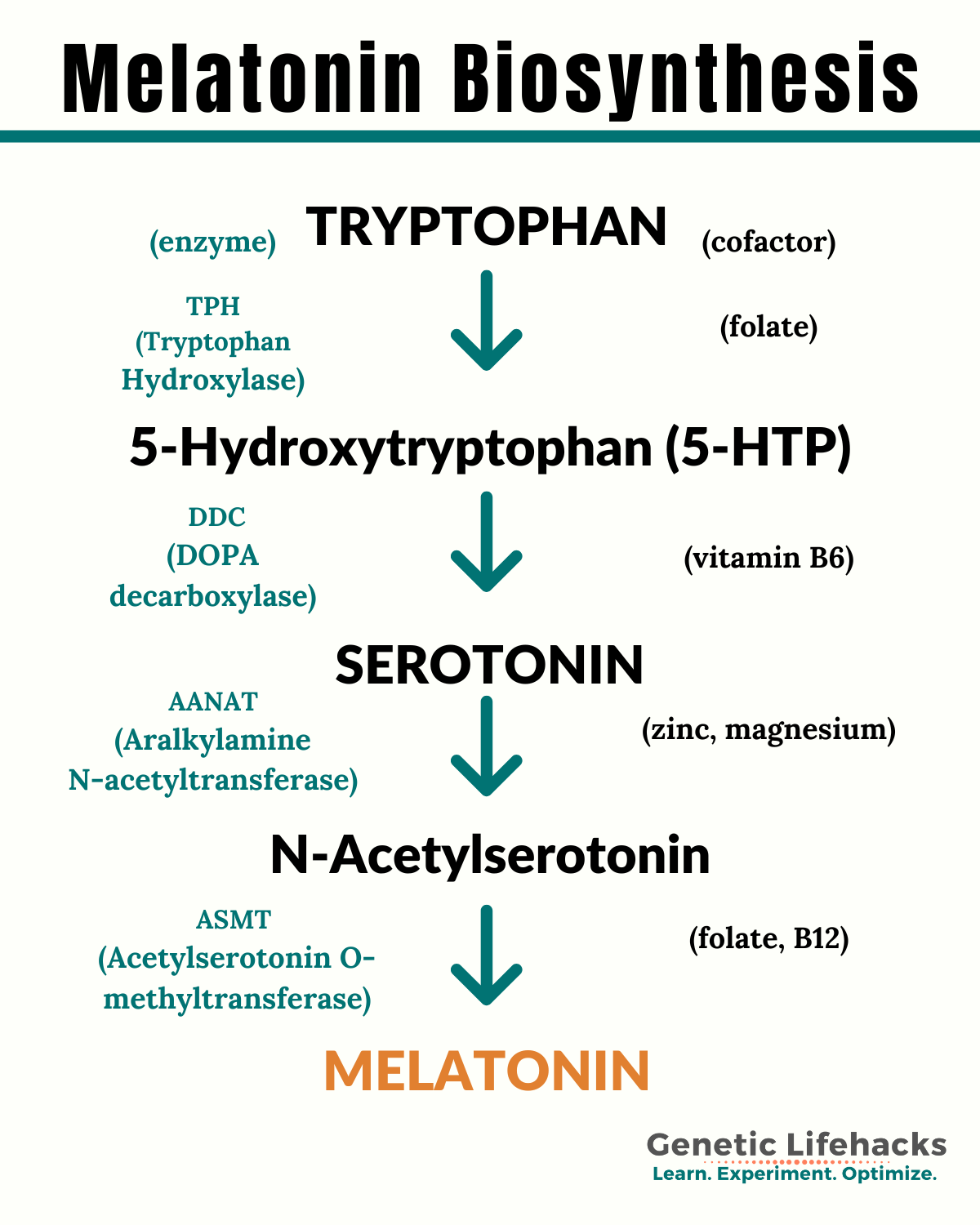
Tryptophan is the precursor amino acid needed for the production of melatonin. Most foods containing protein usually contain tryptophan, and it is readily available in most people’s diets.
Tryptophan converts to serotonin and then into melatonin in a multi-step process. Along the way, several cofactors are needed in this process, including folate, B6, B12, and possibly zinc and magnesium.[ref][ref]
Pineal Gland Melatonin Production
The pineal gland is a tiny endocrine gland in the brain, and pretty much all it does is produce melatonin. Rene Descartes, a 17th-century scientist and philosopher described the pineal gland as “the principal seat of the soul and the place in which all our thoughts are formed.”[ref]
Melatonin can be created inside cells in other organs as well, and it can act as an intracellular antioxidant.[ref] But the majority of melatonin production happens at night and is released by the pineal gland into circulation.
The ‘at night’ part is important. There are two things controlling melatonin production: the circadian clock and light from the environment. The suppression of melatonin synthesis in the pineal gland occurs when light hits the retina of the eye. Specifically, light in the blue wavelengths (around 480nm) activates a non-image-forming photoreceptor called melanopsin, which sends a signal to reduce melatonin production. The lack of 480nm light allows melatonin production to happen in large amounts in the pineal gland.[ref]

The pineal gland, aging, and melatonin production:
As we age, the pineal gland begins to calcify and produce less melatonin at night. This is a downhill slope from adolescence onward. The amount of uncalcified pineal gland volume predicts the amount of melatonin produced at night.[ref]
What is supplemental melatonin useful for?
If we all are destined to produce less melatonin with aging, the question becomes whether or not supplemental melatonin is beneficial.
Melatonin for sleep: regulating circadian rhythm
Let’s get “sleep” out of the way first as a topic since this is what most people think of in regard to melatonin.
Melatonin is often promoted as a supplement to take when you can’t sleep — advertised as the sleep hormone. A review of 35 randomized controlled trials showed that melatonin helps a little with sleep-onset insomnia but that it isn’t a huge effect.[ref]
The exception to the ‘not a huge effect’ is for people who have delayed-sleep phase disorder. For this minority of people, supplemental melatonin can have a significant effect on shifting the timing of sleep and decrease sleep latency significantly.[ref]
Additionally, melatonin helps sleep quality and insomnia in elderly people.[ref]
Melatonin for Alzheimer’s Prevention
Melatonin is linked to Alzheimer’s disease in several important ways:
- Pineal calcification is greater in Alzheimer’s patients than in age-matched controls without dementia.[ref]
- There are decreased melatonin receptors (MT1 and MT2) in the brain regions of people with Alzheimer’s disease.[ref]
- Decreased melatonin production is found in Alzheimer’s patients in comparison to age-matched controls.[ref]
- A melatonin receptor (MT1) variant is linked both to fewer melatonin receptors in the brain and to an increased risk of Alzheimer’s disease.[ref]
Using supplemental melatonin as part of an Alzheimer’s prevention strategy has emerging research to back it up. For instance, melatonin as a free radical scavenger reduces amyloid-beta production. Additionally, circadian rhythm impacts amyloid-beta production, so melatonin acting to set circadian rhythm is also important.[ref]
In a clinical trial of people already in the early stages of Alzheimer’s disease, supplemental melatonin (timed-release, 2mg) slowed the cognitive decline.[ref]
Related article: How to check your genetic data for Alzheimer’s APOE status
Melatonin and your immune system
When it comes to an immune response, balance is key. You want the body to strongly fight off a pathogen, killing off nasty bacteria or viruses. But… you don’t want too strong of an immune response (or too long of a response), resulting in damage to your own cells. Melatonin modulates the immune system response.
Your immune response varies according to your circadian rhythm. In general, your body is primed for an immune system response during the day, with fewer immune system cells produced at night.[ref]
Research shows that melatonin stimulates the production of several types of immune system cells, including natural killer cells and CD4+ cells. Both of these decline with age (along with melatonin.) Supplemental melatonin, therefore, may help to enhance immune function in older people.[ref]
Importantly, though, melatonin also acts to modulate the immune response. When the immune response is overactive, melatonin reduces inflammatory mediators and neutrophil infiltration.[ref]
Viral infections and melatonin:
A recent study showed that people taking supplemental melatonin were 28% less likely to test positive for COVID-19.[ref]
In addition to supporting the immune system, melatonin may interact with one of the proteins in the SARS-CoV-2 virus.[ref] A network-based study also predicts that melatonin should decrease the risk of positive COVID-19 cases.[pre-print] Placebo-controlled trials should tell us more soon about whether melatonin reduces SARS-CoV-2 infections. On-going clinical trials are investigating oral melatonin supplements as a preventative for COVID-19.[ref][ref] In Europe, IV melatonin is being investigated for use in the ICU with COVID patients.[ref][ref] A 2024 placebo controlled trial found that melatonin, along with a mixture of vitamins including zinc, was effective in treating the symptoms of COVID-19 and “accelerating its disappearance” when taken daily. [ref]
Other studies point to the benefits of supplemental melatonin in viral infections as well. A clinical trial shows melatonin plus magnesium, phosphate, and fatty acids is slightly more effective for herpes simplex 1 than standard medication.[ref] Animal and cell-based studies show melatonin to be beneficial in viral myocarditis and RSV infections.[ref][ref][ref][ref]
Related article: Melatonin Research for COVID-19
Melatonin for Osteoporosis:
Melatonin is also important for healthy bone mass. Animal studies show that reduced pineal gland production of melatonin causes low bone mass and that a deficiency of the MT2 melatonin receptor also causes low bone mass. The decrease in bone mass is due to decreased osteoblasts, which form new bone.[ref]
Animal studies show that supplemental melatonin decreases normal ‘post-menopausal’ bone loss.[ref]
The effects of melatonin, though, may be more long-term rather than a quick turnaround. A six-month-long study of perimenopausal women showed that 3mg of melatonin nightly did not statistically affect bone density scores.[ref]
A year-long clinical trial in postmenopausal women with osteopenia found that melatonin did increase bone mineral density (BMD). Interestingly, the increase seemed dependent on the dose. Women taking 3mg of melatonin per night increased femoral BMD by 2.3%, which was greater than the 0.5% increase in the 1mg/day group. Both supplement groups, though, outperformed the placebo group.[ref]
Related article: Osteoporosis Genes and Prevention Strategies
Dental diseases:
Melatonin acts both in bone health for the jaw and as an anti-inflammatory to decrease periodontal inflammation.
In periodontal disease (inflammation of the gums), there is an inverse correlation between melatonin levels in the saliva and the degree of inflammation. Additionally, salivary melatonin levels are higher (on average) in people without gum disease, as compared to people with periodontitis or gingivitis.[ref][ref]
Melatonin is also important in jaw bone health. Numerous animal studies clearly show that melatonin supplementation helps to increase bone growth around implants.[ref]
A clinical trial found that 6mg of supplemental melatonin decreased inflammation (IL-6) and decreased gum bleeding in type 2 diabetics with periodontal disease.[ref]
Related article: Gum Disease and Your Genes
Migraine prevention: is melatonin as good as prescription drugs?
A placebo-controlled clinical trial compared melatonin to amitriptyline (prescription migraine med) for migraine prevention. The study participants took 3mg of melatonin nightly for 4 weeks. Results showed melatonin reduced migraine frequency by 50% performing slightly better than amitriptyline with fewer side effects.[ref] Similar results were found when comparing melatonin to valproate, as well.[ref]
Related article: Using your genetic data to prevent migraines
Depression, circadian rhythm, melatonin:
Circadian rhythm disruption can be at the root of depression, and many circadian rhythm genetic variants increase the risk of depression and bipolar disorder. (Read more here). But how does melatonin impact depression?
Exposure to light at night, even dim levels of light when sleeping, can reduce melatonin production. Dim light at night significantly increases the risk of depression in older adults.[ref]
A prescription antidepressant that binds to the melatonin receptor, agomelatine, is an approved depression and anxiety medication in Europe and Australia.[ref]
What about using melatonin supplements to treat depression? The clinical trial results are all over the place, with some showing it to be effective and others showing no difference from a placebo.[ref]
Related article: Circadian rhythm genes and depression
Reducing acid reflux:
Research shows that people with gastric reflux (heartburn, GERD) have lower levels of melatonin on average compared to healthy controls.[ref][ref]
Will supplemental melatonin help with heartburn?
- A controlled trial tested the benefits of melatonin supplements in people who suffer from GERD. The trial compared a control group to three trial groups: melatonin alone, omeprazole alone, or a combo of melatonin and omeprazole. The combination of melatonin (3mg) and omeprazole worked more quickly to alleviate symptoms (4 weeks). Importantly, though, after 8 weeks of melatonin (3 mg, alone) supplement, all participants had eliminated heartburn symptoms.[ref]
- Another randomized study found that people using a combination of melatonin with l-tryptophan and B vitamins had a complete reversal of GERD after 40 days. This combination was more effective than the omeprazole (20 mg) arm of the trial.[ref]
Mitochondrial function depends on melatonin:
Mitochondria produce the energy stored as ATP, which drives cellular function. The mitochondria can produce melatonin for use within the cell. Melatonin acts as a free-radical scavenger, regulating free radical generation in the mitochondria.[ref]
Cell studies show that melatonin stops mitochondrial fission while enhancing mitophagy (clearance of damaged mitochondria) in liver cells.[ref] In brain cells, “melatonin supplementation reduces cell death and restores mitochondrial function through the regulation of autophagy.”[ref] When challenged with viral-induced liver failure, melatonin modulates mitophagy, preserving mitochondrial function when needed.[ref][ref]
Additional clinical trials of supplemental melatonin:
- Atopic dermatitis: A clinical trial in kids with atopic dermatitis (eczema) found that 3mg of melatonin per night reduced the rash significantly. It also helped the kids fall asleep 21 minutes faster.[ref]
- Blood glucose levels: A recent meta-analysis shows that supplemental melatonin reduces fasting blood glucose levels. Additionally, it increases insulin sensitivity, but it doesn’t influence overall insulin levels.[ref]
- Blood pressure: Another meta-analysis pooled the data from clinical trials on blood pressure and melatonin supplementation. The results showed that melatonin supplements reduce blood pressure (a little) in people who have high blood pressure.[ref]
- DNA damage: A trial of 20mg/day of melatonin in high-intensity interval training athletes decreased DNA damage.[ref]
Cancer and melatonin:
Common sense note: If you have questions about cancer, talk with your doctor. While there are likely cancer prevention benefits from melatonin, it is not going to cure cancer (even if you read that it would on the Facebook).
Breast cancer: Numerous studies have looked at the link between higher melatonin levels and decreased breast cancer risk. These studies show several different mechanisms through which higher melatonin levels protect against the risk of breast cancer. For example, exposure to light at night, which reduces endogenous melatonin production, is a well-studied risk factor for breast cancer. Additionally, studies show that women with ER+ breast cancers have lower nocturnal plasma melatonin concentrations on average. One more way that melatonin protects against breast cancer is by protecting against the harmful effects of cadmium, which acts as a metalloestrogen to increase the risk of breast cancer.[ref][ref]
Lung cancer: Exogenous melatonin is being studied as a combination treatment with chemotherapy for lung cancer. The benefits may stem from melatonin’s ability to inhibit metastasis as well as slow tumor growth.[ref]
Cancer in general: Melatonin acts as a free radical scavenger, decreasing oxidative stress and preventing damage to DNA. DNA damage in the wrong place can cause cancer. Thus, in general, melatonin could decrease the initiation of cancer-causing mutations. Additionally, melatonin acts through the MT1 receptor at night to protect against double-stranded DNA breaks. Here is a great overview of all of the research on melatonin reducing DNA damage from radiation, reactive oxygen species, and other free radicals.
The World Health Organization lists light at night as a probable carcinogen. The increase in cancer due to light at night is, in part, due to the reduction in melatonin.
Melatonin supplements: getting into the details
In the US and Canada, melatonin is considered a dietary supplement and is available over the counter. In other countries, such as the UK, it is considered a drug, and you may need a prescription.
More is not always better:
When you look for melatonin supplements, you are going to find a wide range of products. Supplements come in 0.3mg (300 mcg) to 10 mg ranges. Most studies seem to use 1 – 3 mg doses, but the overall range is from 0.1mg to 50mg.[ref]
Since your need for melatonin increases with age, there is no one-size-fits-all answer here… Instead, let’s look at how quickly metabolization occurs and the different formulations available, and you can experiment to find out what works best for you.
The half-life of supplemental melatonin:
A study in young adult males looked at the pharmacokinetics of a 10 mg oral dose of supplemental melatonin. The results showed that the absorption of oral melatonin is pretty quick, with melatonin levels rising after 6 minutes. Maximum absorption was reached at 40 minutes, and the half-life for elimination was 53 minutes.[ref]
Here is a graph of how quickly melatonin is metabolized:[CC license ref]
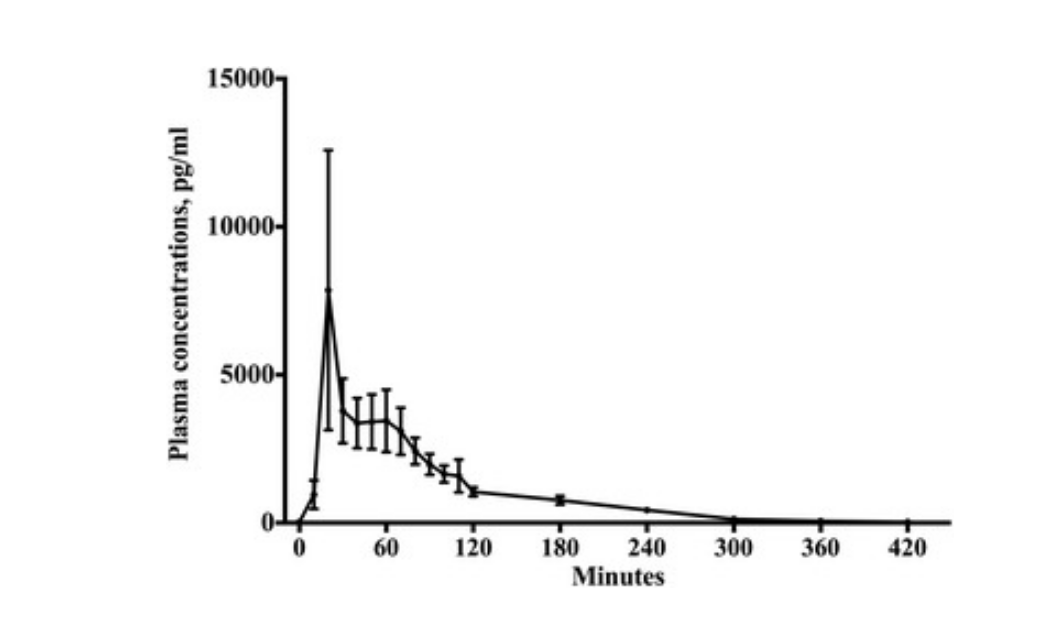
Timed-release vs. immediate-release melatonin:
With the half-life of oral melatonin being less than an hour, you may want to consider a timed-release (sustained-release) melatonin supplement instead. This should better mimic normal, overnight melatonin production.
Timed-release melatonin (2mg dose) has been shown in a double-blind, placebo-controlled clinical trial to decrease sleep latency (the time it takes to get to sleep) in people aged 55+. Additionally, timed-release melatonin improved sleep quality for all age groups (18-80).[ref]
Metabolism of melatonin:
The CYP family of enzymes breaks down or metabolizes drugs (medications, supplements) as well as substances produced in the body. In metabolizing melatonin, the enzymes CYP1A1, CYP1A2, and CYP1B1 can all be used. Additionally, CYP2C19 plays a minor role in metabolism.[ref] While variants that slow the function are common in all of those CYP genes, it is less likely that a variant in any single gene will cause issues with melatonin due to the ubiquity of all three CYP enzymes.
Melatonin can also be used and broken down in reactions involving neutralizing reactive oxygen species (ROS), and it can be metabolized in the mitochondria using cytochrome C. In the brain, the metabolism of melatonin uses IDO, also important in the kynurenine pathway. Interestingly, some of the metabolites of melatonin also are important as antioxidants that interact with ROS.[ref]
What about the safety of melatonin supplements?
Side effects reported for melatonin supplements:
Anecdotal side effects include grogginess in the morning after larger doses of melatonin and a general hangover-type feeling.
The majority of clinical trials report no adverse effects from melatonin, but this likely refers to significant effects. The trials that do include minor, short-lived adverse events show melatonin supplements may be linked to fatigue, mood, or ‘neurocognitive performance’ for some people. These events were linked to dosage and timing.[ref] In other words, if you take too much melatonin or take it too late at night, the next morning you could be foggy and grumpy.
Will you stop producing melatonin if you take supplemental melatonin?
The answer here seems to be ‘no’. Studies show no rebound effects or withdrawal symptoms from stopping supplemental melatonin.
- One study that looked at 6 months of supplemental timed-release melatonin found no withdrawal symptoms and no rebound insomnia when melatonin was stopped.[ref]
- Other studies on longer-term (10+ years) melatonin supplements also found no adverse effects on sleep when stopping melatonin.[ref]
Quality of melatonin supplements:
Not all supplements contain the amount that they state on the label. Labdoor is a company that tests supplements off the shelf to see if they contain what is on the label and whether there are any impurities in the product. Check out Labdoor’s ranking for melatonin supplements. (I have no affiliation with this company – I just like what they are doing.)
Medication interactions and pregnancy:
Medication interactions with epilepsy.
Melatonin may decrease blood pressure in people with hypertension, so it is possible that you could have an interaction with blood pressure-lowering medications.[ref]
If you are pregnant or breastfeeding — talk to your doctor, of course, but in general, melatonin supplements are not recommended. Melatonin does cross the placenta, and it is important for the baby. Instead, you may be better off blocking blue light at night to increase your natural melatonin levels rather than supplementing with higher amounts than are normal for your body.[ref]
Melatonin Genotype Report
Not a member? Join here. Membership lets you see your data right in each article and also gives you access to the member’s only information in the Lifehacks sections.
There are several ways that your genes interact with melatonin: through production, cellular receptors, and metabolism.
Below is an overview of some of the studies associated with melatonin-related genetic variants that are available in 23andMe or AncestryDNA data.
Variants related to the production of melatonin:
AANAT gene: The alkylamine N-acetyltransferase (AANAT) gene controls the rhythmic production of melatonin by the pineal gland.
Check your genetic data for rs28936679 (23andMe v4 only):
- A/A: rare, linked to delayed sleep phase disorder[ref]
- A/G: rare, may cause delayed phase sleep disorder
- G/G: typical
Members: Your genotype for rs28936679 is —.
Check your genetic data for rs3760138 (AncestryDNA):
- G/G: decreased melatonin; increased risk of breast cancer[ref], increased risk of lupus[ref], possibly increased risk of depression[ref]
- G/T: typical risk
- T/T: typical
Members: Your genotype for rs3760138 is —.
TPH2 Gene: The TPH2 gene codes for the rate-limiting enzyme involved in the conversion of tryptophan to serotonin, which can then be converted to melatonin. The link between TPH2 and melatonin levels is indirect, but I’ve included it here to illustrate the connection between melatonin precursors and disrupted circadian rhythm.[ref][ref]
Check your genetic data for rs4290270 (23andMe v4; AncestryDNA):
- T/T: increased risk of waking early, increased risk of depression[ref][ref]
- A/T: probably a slightly increased risk of waking early, depression (this is the most common genotype)
- A/A: typical
Members: Your genotype for rs4290270 is —.
Check your genetic data for rs4570625 (23andMe v4, v5; AncestryDNA):
- G/G: less TPH2 function[ref], more likely to achieve depression remission with escitalopram*[ref]
- G/T: higher TPH2
- T/T: higher TPH2, less depression[ref]
Members: Your genotype for rs4570625 is —.
*Escitalopram is an antidepressant that acts on the circadian system.[ref]
Melatonin receptor variants:
MTNR1B gene: This gene codes for the MT2 melatonin receptor.
Check your genetic data for rs10830963 (23andMe v4, v5; AncestryDNA):
- G/G: linked to a higher risk of diabetes, gestational diabetes[ref][ref][ref][ref], increased fasting glucose – don’t eat dinner late[ref]
- C/G: linked to a higher risk of diabetes, increased fasting glucose – don’t eat dinner late
- C/C: typical
Members: Your genotype for rs10830963 is —.
Check your genetic data for rs1387153 (23andMe v4, v5; AncestryDNA):
- T/T: increased fasting glucose, increased risk of gestational diabetes[ref]
- C/T: somewhat increased fasting glucose
- C/C: typical
Members: Your genotype for rs1387153 is —.
MTNR1A gene: This gene codes for the MT1 melatonin receptor.
Check your genetic data for rs2375801 (23andMe v4):
- C/C: increased risk of cancer metastasis (liver)[ref]
- C/T: increased risk of cancer metastasis (liver)
- T/T: typical
Members: Your genotype for rs2375801 is —.
Check your genetic data for rs6553010 (23andMe v4, AncestryDNA):
- A/A: increased risk of cancer metastasis (liver)[ref]
- A/G: increased risk of cancer metastasis (liver)
- G/G: typical
Members: Your genotype for rs6553010 is —.
Check your genetic data for rs12506228 (23andMe v4, v5; AncestryDNA):
- A/A: likely fewer melatonin receptors in the brain, a greater impact from working the night shift, increased risk of Alzheimer’s[ref][ref]
- A/C: somewhat fewer melatonin receptors, somewhat impacted from light at night, increased risk of Alzheimer’s
- C/C: typical MTNR1A variant
Members: Your genotype for rs12506228 is —.
Note: As far as I can find, no research exists showing the CYP enzymes involved in melatonin metabolism have an effect on supplement melatonin.
Lifehacks for increasing your melatonin production:
While supplements are a nice option, you may also want to consider ways to raise your own natural production of melatonin. Producing melatonin endogenously is likely a better option since it rises and falls at the right time in sync with your circadian rhythm.
What can you do to increase production of melatonin at night?
The rest of this article is for Genetic Lifehacks members only. Consider joining today to see the rest of this article.
Related Articles and Genes:
Why light at night increases the risk for cancer
The World Health Organization listed ‘light at night’ as a possible carcinogen in 2007. Let’s let that sink in for a minute… On the same list of possible carcinogens that includes formaldehyde, aflatoxin, and the HPV virus is something as innocent as artificial light at night.
Serotonin: How your genes affect this neurotransmitter
There is a lot more to this molecule than most of us realize! This article covers the way that serotonin is made in the body, the transport of serotonin, and the receptors needed to complete the pathway.
DEC2: Are you a genetic short sleeper?
A rare mutation in the DEC2 gene causes some people to need about an hour and a half less sleep each night. People with the mutation average 6 to 6.5 hours of sleep.