Key takeaways:
~ Mushroom intolerance symptoms, such as intestinal issues, may stem from your genes.
~ Ergothionine is a natural compound found in mushrooms and fungi that has antioxidant properties, which are good in the right amount.
~ For people with gut issues, such as IBD, variants in the ergothioneine transporter cause too much ergothioneine to be absorbed, exacerbating IBD symptoms.
~ Ergothionine is found in a few other foods in addition to mushrooms, and a natural supplement may help.
Mushroom Intolerance: Intestinal Sensitivity
I love mushrooms and can eat them in abundance.
But I know a lot of people dislike mushrooms – perhaps for a genetic reason? For some people with intestinal problems and a specific genetic variant, mushrooms can exacerbate these problems.
Mushrooms and Crohn’s Disease (IBD)
Crohn’s disease is a serious inflammatory disorder affecting the lining of the intestines. It can cause abdominal pain, fatigue, diarrhea, and weight loss. For some people, it is a chronic condition, but for others, it may flare up only periodically.
An interesting study published in the British Journal of Nutrition looked at some of the foods that trigger intestinal issues in people with inflammatory bowel diseases (mainly Crohn’s).
The study participants were a group of New Zealand Crohn’s patients and a control group without Crohn’s. The researchers were looking at the interaction between foods, disease symptoms, and genetics.[ref]
The top foods found to aggravate intestinal symptoms were corn and mushrooms. Corn is a known allergen and a general trigger for a lot of people. The mushroom connection, though, was linked to a specific compound in mushrooms and a specific gene.
The researchers linked the ‘intolerant of mushrooms’ group to a genetic variant of the OCTN1 gene, which in previous studies had links to an increased risk of Crohn’s disease (without a reason why).
The OCTN1 / SLC22A4 gene:
The OCTN1 gene (now known as SLC22A4) codes for a transporter of organic cations, which means it moves solutes with a positive charge across the plasma membrane.
Specifically, SLC22A4 moves ergothioneine, a compound available abundantly in mushrooms, across the plasma membrane.
Additionally, the SLC22A4 transports gabapentin, and the variant below impacts the clearance of gabapentin.[ref]
Related article: GABA levels: Genetic variants that impact this inhibitory neurotransmitter
What is ergothioneine?
Ergothioneine has been the subject of many research studies lately due to its antioxidant properties and potential role in helping with cardiovascular disease. Researchers are looking at it as a positive factor with the potential for use as a supplement. Which may be great – for some people…
Ergothioneine is a compound naturally synthesized by bacteria and fungi. We naturally consume ergothioneine in our diet in small quantities. Specific soil fungi and bacteria produce ergothioneine, which is taken up by the roots of some plants.
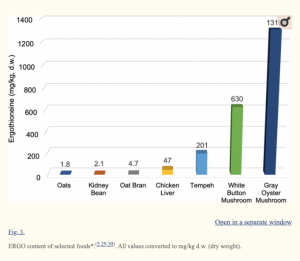
Our main food source for ergothioneine is mushrooms (white button, shiitake, portobello, and oyster). Other food sources that contain some ergothioneine include tempeh, liver, black and red beans, and oat bran.[ref] It is interesting to note that in the Crohn’s study referenced above, other foods on the top offenders’ list included baked beans, chickpeas, and dried beans.
The variant of SLC22A4 linked to Crohn’s disease in the study referenced above, and also to mushroom intolerance for those with Crohn’s disease, causes a gain of function with a 50% increased transport of ergothioneine (ET).
Even though we often think of antioxidants as something to consume in abundance, the study explains: “high levels of ET might lead to an antioxidant overload in red blood cells or epithelium, leading to pro-oxidant effects and/or imbalance in immune reaction. An alternative possibility might involve effects on pro-inflammatory cytokines or heat shock protein 70”.[ref]
Ergothioneine, mushrooms, and adaptation of an agricultural diet?
Researchers who look at evolutionary genetic traits find that certain genetic variants are linked to humans switching from hunter/gatherers to a more agriculture-based society. Some researchers theorize that this genetic variant in the SLC22A4 gene is an adaptation in European populations to protect against ergothioneine deficiency in agriculture-based diets.[ref]
Related article: Inflammatory Bowel, Crohn’s Disease, and Gut Microbes
Mushroom Intolerance Genotype Report
Access this content:
An active subscription is required to access this content.
Lifehacks:
Carrier of the rs1050152 T-allele? If you have intestinal issues, and especially if you have an inflammatory bowel disease, you may want to try cutting out foods high in ergothioneine for a period of time to see if it impacts your symptoms.
Which foods contain ergothioneine?
Access this content:
An active subscription is required to access this content.
Related Genes and Topics:
Histamine Intolerance: Genetic Report, Supplements, and Real Solutions
While FODMAPs works for a lot of people with IBS, it doesn’t work for everyone. Genetics research explains why some people need a different dietary approach to IBS.
Originally published 06/2017. Updated 11/2019.