Vaccines have been around in one form or another for about 200 years. They have saved millions of lives and prevented long-term suffering from diseases like tuberculosis and polio. While there is no denying that the human population benefits from vaccines, there are questions surrounding vaccinations and autoimmune diseases. On the one hand, certain vaccines may slightly increase the absolute risk of autoimmune diseases in susceptible individuals. The flip side is that some vaccines may protect against specific autoimmune diseases.
This is not a cut-and-dried topic, so stick with me through the ins and outs of the research. Note that no research yet shows an impact on autoimmune diseases from the COVID-19 vaccine.
In this article, I’m just bringing together information from research studies — if you have medical questions, please consult your doctor.
Vaccines, Autoimmune Diseases, and Your Immune System
There are various types of vaccines, but the overarching goal is to cause an immune system response to a specific pathogen. Vaccines prompt your body’s immune system to create a reaction – usually involving antibodies or a T-cell response against the virus or bacteria.
Most adverse vaccine events are short-lived and transient, such as not feeling well the next day or having a sore spot where the shot was administered.[ref] But there are rare cases of more severe adverse vaccination reactions.[ref]
Autoimmune diseases and Infections:
Autoimmune diseases arise from the body mistaking a certain cell type for ‘foreign’ rather than ‘self’.
In general, autoimmune diseases are thought to be caused by a combination of genetic susceptibility, immune activation, hormones, and/or environmental trigger.[ref] That ‘trigger’ can be an exposure to toxins, a trauma such as surgery, an altered gut microbiome, pregnancy, or an infection by a virus or bacteria.
So how can a virus or bacterial pathogen cause an autoimmune reaction? Recent research shows that one way is through causing cell death. The immune system clears out the dead cells, but the cells contain both the pathogen’s DNA and the host’s DNA. Therefore, this action triggers an immune response against both pathogen and host DNA.[ref]
Other research shows a pathogen could trigger an autoimmune disease due to molecular mimicry, which could happen if the pathogen antigen is similar to a host antigen.[ref]
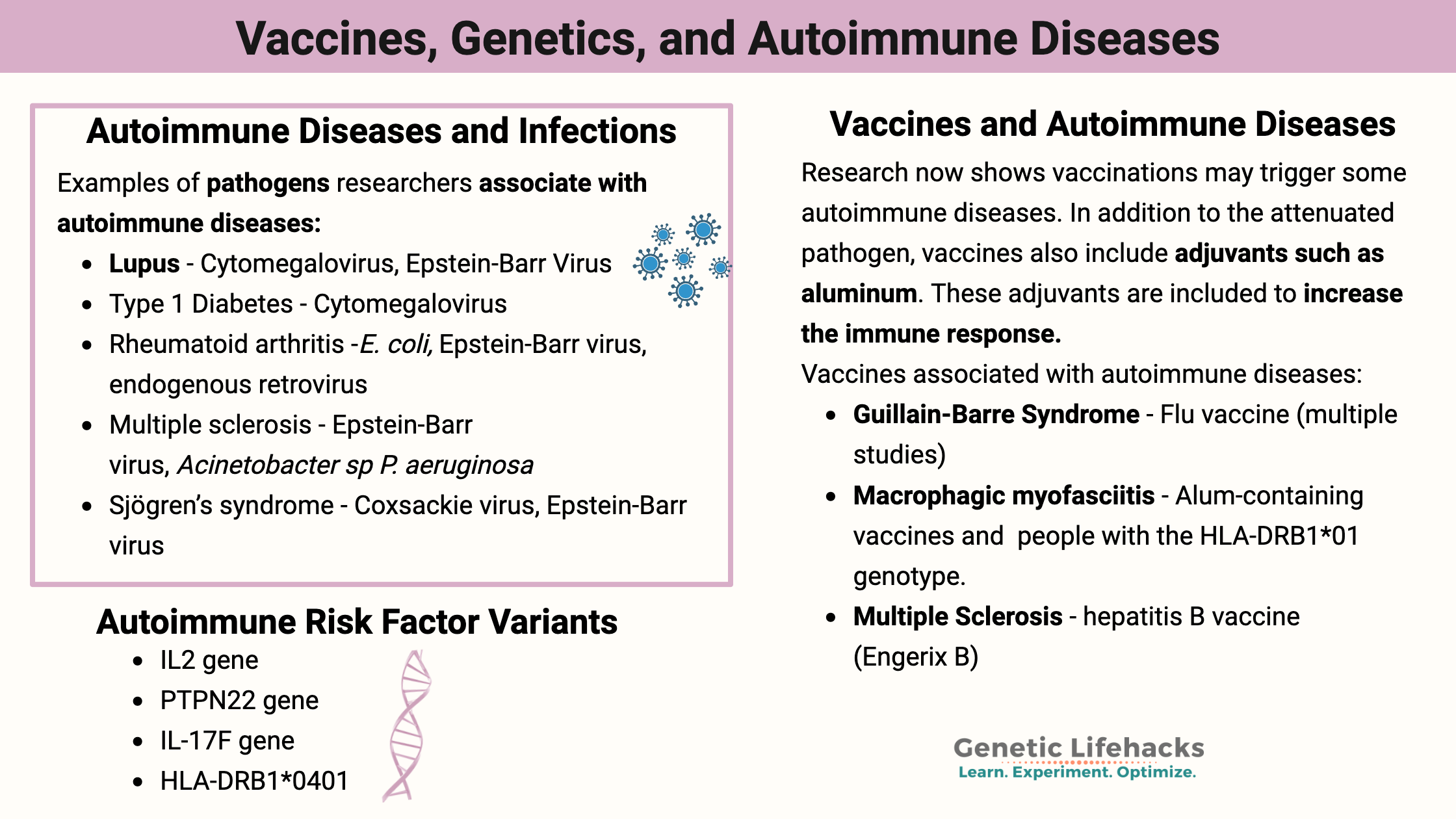
Let me give you some examples of pathogens researchers associate with autoimmune diseases[ref]:
| Autoimmune Disease | Pathogen |
|---|---|
| Lupus | Cytomegalovirus, Epstein-Barr Virus, T. gondii |
| Antiphospholipid syndrome | Epstein-Barr Virus, C. tetani |
| Type 1 Diabetes | Cytomegalovirus, Saccharomyces cerevisiae |
| Rheumatoid arthritis | E. coli, K. pneumoniae, P. mirabilis, Epstein-Barr virus, endogenous retrovirus |
| Multiple sclerosis | Epstein-Barr virus, Acinetobacter sp P. aeruginosa |
| Sjögren’s syndrome | Coxsackie virus, Epstein-Barr virus |
Related article: Epstein-Barr Virus
Keep in mind that the pathogen alone likely is not the single cause of the autoimmune disease. Instead, it is the pathogen along with genetic susceptibility, environmental factors, and possibly epigenetic changes.[ref]
Autoimmune diseases triggered by vaccinations:
Research now shows vaccinations may trigger some autoimmune diseases. Again – this is not a common event, and it is likely due to multiple factors, including genetics, epigenetics, and environment.
In addition to the attenuated pathogen, vaccines also include adjuvants such as aluminum. These adjuvants are included to increase the immune response. Adjuvants can increase immune response by enhancing the injection site reaction, increasing the release of inflammatory cytokines, or translocating the antigens to the lymph nodes.[ref]
Example time: The 2009-2010 flu vaccine caused narcolepsy in genetically susceptible people.
While still a relatively uncommon occurrence, the H1N1 vaccine caused a 5 to 14-fold increase in the risk of narcolepsy in children and teens. Adults had a ~7-fold increase in risk. In addition to the vaccine, all of the narcolepsy patients carried a specific genotype for HLA-DQB1*06:02.[ref][ref][ref] Again, this was a rare convergence of genetic susceptibility, a specific vaccine, and likely unknown environmental factors. While rare (about 1 in 30,000 children), the fact that the flu vaccine was widely used caused many to end up with autoimmune-induced narcolepsy.[ref]
Other autoimmune diseases linked to vaccines include:
- Macrophagic myofasciitis is an autoimmune reaction at the injection site that lasts for months to years. It is triggered by alum-containing vaccines in people with the HLA-DRB1*01 genotype.[ref]
- In the 90s, it was determined that the relative risk of Guillain-Barre Syndrome increased by 4 to 8-fold following the flu vaccine (compared to people getting a tetanus shot). While the relative risk sounds scary, this was a rare vaccine side-effect when looking at the absolute risk.[ref] Guillain-Barre is an autoimmune condition that attacks the myelin sheath on peripheral nerves, eventually leading to whole-body paralysis.
- Another study published in 2009 showed that Guillain-Barre Syndrome risk was increased when receiving either the flu vaccine or hepatitis B vaccine.[ref] Keep in mind that the flu vaccine changes yearly, so the data from the 90s and early 2000s may not be as relevant today.
- One specific hepatitis B vaccine, Engerix B, was shown in a French study to increase the risk of CNS inflammatory demyelination (Multiple Sclerosis).[ref]
- It has been known since the 1960s that the measles vaccine increases the risk of immune thrombocytopenia (an autoimmune condition causing decreased platelets). A 2008 study estimates that for every 40,000 children getting an MMR shot, the vaccine will cause 1 case of autoimmune thrombocytopenia.[ref]
While these examples are real and significant, vaccinations do not trigger autoimmune diseases for most people. Many studies of specific vaccines show no link to an increased risk of autoimmune disease.[ref] For example, a 2020 meta-analysis found no “association between HPV vaccinations, autoimmune diseases, and other rare diseases.” [ref]
One research study on the increased risk of multiple sclerosis after vaccination concluded that “The short-term increase in risk suggests that vaccines may accelerate the transition from subclinical to overt autoimmunity in patients with existing disease.”[ref] In other words, certain vaccines may just accelerate the autoimmune condition in people who are already partly there.
The good side of vaccines: killing cancer & preventing autoimmune diseases
Triggering an autoimmune reaction by a vaccine can be a good thing. One cell type the body needs to kill off is cancer cells. For the past four decades, researchers have known that the BCG vaccine (tuberculosis) causes the body to recognize and kill off bladder cancer cells.[ref][ref]
There are many different vaccines in trials now that specifically target different types of cancer. For example, the live attenuated measles vaccine may also help target glioblastoma cells. Additionally, a poliovirus vaccine is being revamped to target glioblastoma brain tumors.[ref][ref][ref]
Additionally, certain vaccines are linked with a lower risk of autoimmune diseases. Animal studies show that the BCG vaccine protects against type 1 diabetes in genetically susceptible animals. A clinical trial in Italy showed that the BCG vaccine decreased the risk of MS in people with early disease symptoms.[ref]
Research on vaccination safety in people with autoimmune diseases:
If you already have an autoimmune disease, you may wonder if you are at risk for complications from a vaccine. This is something, of course, to talk with your doctor about for your individual circumstances.
You can also check out the CDC guidelines, which, for example, include people with autoimmune diseases who should not get the hepatitis B vaccine.[ref]
Research on specific autoimmune diseases and specific vaccines:
- Trivalent influenza vaccine: A study of 24 patients with either lupus and/or rheumatoid arthritis showed no difference from a healthy control group.[ref]
- Quadrivalent HPV vaccine: A study of 50 patients with lupus found no differences from healthy control in their reaction to the HPV vaccine.[ref]
- Tetanus, hepatitis B, flu: A study of 643 MS patients found no increase in relapse due to vaccinations for tetanus, hep B, or the flu (1993-1997).[ref]
- Live attenuated virus vaccines: Some government health agencies give a general recommendation against live attenuated virus vaccines for people with autoimmune diseases who are on immunosuppressant drugs.[ref]
Autoimmune Diseases and Vaccine Genotype Report:
Access this content:
An active subscription is required to access this content.
Lifehacks:
While there are statistically significant increases in risk for certain autoimmune diseases associated with specific vaccines, the overall or absolute risk is still very low.
Talk with your doctor if you have questions about vaccinations, especially if you have an autoimmune disease. There are specific protocols and standards for vaccinations depending on the autoimmune disease and on certain immune system suppression medications.[ref]
Related Articles and Topics:
IL-17: Chronic Inflammation & Autoimmune Risk with IL17A, IL17F
Guillain-Barré Syndrome: Genetic Risk Factors and Known Triggers
References:
Abbasi, Zahra, et al. “Association of PTPN22 Rs2476601 Polymorphism with Rheumatoid Arthritis and Celiac Disease in Khuzestan Province, Southwestern Iran.” Iranian Biomedical Journal, vol. 21, no. 1, Jan. 2017, pp. 61–66. PubMed Central, https://doi.org/10.6091/.21.1.61.
ACIP Contraindications Guidelines for Immunization | CDC. 14 Apr. 2022, https://www.cdc.gov/vaccines/hcp/acip-recs/general-recs/contraindications.html.
Alhunaidi, Omar, and Alexandre R. Zlotta. “The Use of Intravesical BCG in Urothelial Carcinoma of the Bladder.” Ecancermedicalscience, vol. 13, 2019, p. 905. PubMed, https://doi.org/10.3332/ecancer.2019.905.
Al-Shammari, Ahmed M., et al. “Live Attenuated Measles Virus Vaccine Therapy for Locally Established Malignant Glioblastoma Tumor Cells.” Oncolytic Virotherapy, vol. 3, 2014, pp. 57–68. PubMed, https://doi.org/10.2147/OV.S59037.
Arango, María-Teresa, et al. Infection and Autoimmune Diseases. El Rosario University Press, 2013. www.ncbi.nlm.nih.gov, https://www.ncbi.nlm.nih.gov/books/NBK459437/.
Bin Huraib, Ghaleb, et al. “The Protein Tyrosine Phosphatase Nonreceptor 22 (PTPN22) R620W Functional Polymorphism in Psoriasis.” Clinical Medicine Insights. Arthritis and Musculoskeletal Disorders, vol. 11, 2018, p. 1179544117751434. PubMed, https://doi.org/10.1177/1179544117751434.
Castiblanco, John, and Juan-Manuel Anaya. “Genetics and Vaccines in the Era of Personalized Medicine.” Current Genomics, vol. 16, no. 1, Feb. 2015, pp. 47–59. PubMed Central, https://doi.org/10.2174/1389202916666141223220551.
Chung, Ill-Min, et al. “Rheumatoid Arthritis: The Stride from Research to Clinical Practice.” International Journal of Molecular Sciences, vol. 17, no. 6, June 2016, p. 900. PubMed Central, https://doi.org/10.3390/ijms17060900.
Crabtree, Juliet N., et al. “Autoimmune Variant PTPN22 C1858T Is Associated With Impaired Responses to Influenza Vaccination.” The Journal of Infectious Diseases, vol. 214, no. 2, July 2016, pp. 248–57. PubMed Central, https://doi.org/10.1093/infdis/jiw126.
Dhiman, Neelam, et al. “Associations between Measles Vaccine Immunity and Single-Nucleotide Polymorphisms in Cytokine and Cytokine Receptor Genes.” The Journal of Infectious Diseases, vol. 195, no. 1, Jan. 2007, pp. 21–29. PubMed, https://doi.org/10.1086/510596.
France, Eric K., et al. “Risk of Immune Thrombocytopenic Purpura after Measles-Mumps-Rubella Immunization in Children.” Pediatrics, vol. 121, no. 3, Mar. 2008, pp. e687-692. PubMed, https://doi.org/10.1542/peds.2007-1578.
Geier, Mark R., et al. “Influenza Vaccination and Guillain Barre Syndrome.” Clinical Immunology (Orlando, Fla.), vol. 107, no. 2, May 2003, pp. 116–21. PubMed, https://doi.org/10.1016/s1521-6616(03)00046-9.
Gorman, Jennifer D., et al. “Particular HLA-DRB1 Shared Epitope Genotypes Are Strongly Associated with Rheumatoid Vasculitis.” Arthritis and Rheumatism, vol. 50, no. 11, Nov. 2004, pp. 3476–84. PubMed, https://doi.org/10.1002/art.20588.
Hallberg, Pär, et al. “Pandemrix-Induced Narcolepsy Is Associated with Genes Related to Immunity and Neuronal Survival.” EBioMedicine, vol. 40, Feb. 2019, pp. 595–604. PubMed, https://doi.org/10.1016/j.ebiom.2019.01.041.
Israeli, Eitan, et al. “Macrophagic Myofaciitis a Vaccine (Alum) Autoimmune-Related Disease.” Clinical Reviews in Allergy & Immunology, vol. 41, no. 2, Oct. 2011, pp. 163–68. PubMed, https://doi.org/10.1007/s12016-010-8212-4.
Lamm, D. L., et al. “Bacillus Calmette-Guerin Immunotherapy of Superficial Bladder Cancer.” The Journal of Urology, vol. 124, no. 1, July 1980, pp. 38–40. PubMed, https://doi.org/10.1016/s0022-5347(17)55282-9.
Langer-Gould, Annette, et al. “Vaccines and the Risk of Multiple Sclerosis and Other Central Nervous System Demyelinating Diseases.” JAMA Neurology, vol. 71, no. 12, Dec. 2014, pp. 1506–13. PubMed, https://doi.org/10.1001/jamaneurol.2014.2633.
Mikaeloff, Yann, et al. “Hepatitis B Vaccine and the Risk of CNS Inflammatory Demyelination in Childhood.” Neurology, vol. 72, no. 10, Mar. 2009, pp. 873–80. PubMed, https://doi.org/10.1212/01.wnl.0000335762.42177.07.
Mok, Chi Chiu, et al. “Immunogenicity and Safety of a Quadrivalent Human Papillomavirus Vaccine in Patients with Systemic Lupus Erythematosus: A Case–Control Study.” Annals of the Rheumatic Diseases, vol. 72, no. 5, May 2013, pp. 659–64. ard.bmj.com, https://doi.org/10.1136/annrheumdis-2012-201393.
Pabalan, Noel, et al. “Association of the Protein Tyrosine Phosphatase Non-Receptor 22 Polymorphism (PTPN22) with Endometriosis: A Meta-Analysis.” Einstein (Sao Paulo, Brazil), vol. 15, no. 1, Mar. 2017, pp. 105–11. PubMed, https://doi.org/10.1590/S1679-45082017RW3827.
Pearson, Frances E., et al. “Human CLEC9A Antibodies Deliver Wilms’ Tumor 1 (WT1) Antigen to CD141 + Dendritic Cells to Activate Naïve and Memory WT1‐specific CD8 + T Cells.” Clinical & Translational Immunology, vol. 9, no. 6, Jan. 2020. DOI.org (Crossref), https://doi.org/10.1002/cti2.1141.
Rasmussen, H. B., et al. “Additive Effect of the HLA-DR15 Haplotype on Susceptibility to Multiple Sclerosis.” Multiple Sclerosis (Houndmills, Basingstoke, England), vol. 7, no. 2, Apr. 2001, pp. 91–93. PubMed, https://doi.org/10.1177/135245850100700203.
Saitoh, Takayuki, et al. “Interleukin-17F Gene Polymorphism in Patients with Chronic Immune Thrombocytopenia.” European Journal of Haematology, vol. 87, no. 3, Sept. 2011, pp. 253–58. PubMed, https://doi.org/10.1111/j.1600-0609.2011.01651.x.
Sarkanen, Tomi, et al. “Narcolepsy Associated with Pandemrix Vaccine.” Current Neurology and Neuroscience Reports, vol. 18, no. 7, June 2018, p. 43. PubMed, https://doi.org/10.1007/s11910-018-0851-5.
Silber, Michael H. “Autoimmune Sleep Disorders.” Handbook of Clinical Neurology, vol. 133, 2016, pp. 317–26. PubMed, https://doi.org/10.1016/B978-0-444-63432-0.00018-9.
Souayah, Nizar, et al. “Guillain-Barré Syndrome after Vaccination in United States: Data from the Centers for Disease Control and Prevention/Food and Drug Administration Vaccine Adverse Event Reporting System (1990-2005).” Journal of Clinical Neuromuscular Disease, vol. 11, no. 1, Sept. 2009, pp. 1–6. PubMed, https://doi.org/10.1097/CND.0b013e3181aaa968.
Stowe, Julia, et al. “Reassessment of the Risk of Narcolepsy in Children in England 8 Years after Receipt of the AS03-Adjuvanted H1N1 Pandemic Vaccine: A Case-Coverage Study.” PLoS Medicine, vol. 17, no. 9, Sept. 2020, p. e1003225. PubMed, https://doi.org/10.1371/journal.pmed.1003225.
Thompson, Susan D., et al. “The Susceptibility Loci Juvenile Idiopathic Arthritis Shares with Other Autoimmune Diseases Extend to PTPN2, COG6, and ANGPT1.” Arthritis and Rheumatism, vol. 62, no. 11, Nov. 2010, pp. 3265–76. PubMed, https://doi.org/10.1002/art.27688.
Traylor, Matthew, et al. “Genetic Associations with Radiological Damage in Rheumatoid Arthritis: Meta-Analysis of Seven Genome-Wide Association Studies of 2,775 Cases.” PloS One, vol. 14, no. 10, 2019, p. e0223246. PubMed, https://doi.org/10.1371/journal.pone.0223246.
VAERS – Data. https://vaers.hhs.gov/data.html. Accessed 25 Aug. 2022.
Watad, A., et al. “Autoimmune/Inflammatory Syndrome Induced by Adjuvants (Shoenfeld’s Syndrome) – An Update.” Lupus, vol. 26, no. 7, June 2017, pp. 675–81. DOI.org (Crossref), https://doi.org/10.1177/0961203316686406.
Yan, Ni, et al. “Association of Interleukin-17A and -17F Gene Single-Nucleotide Polymorphisms with Autoimmune Thyroid Diseases.” Autoimmunity, vol. 45, no. 7, Nov. 2012, pp. 533–39. PubMed, https://doi.org/10.3109/08916934.2012.702814.
Yousefi, Azizollah, et al. “Autoimmune Hepatitis Association with Single Nucleotide Polymorphism of Interleukin-2, but Not Interferon-Gamma.” Clinics and Research in Hepatology and Gastroenterology, vol. 42, no. 2, Apr. 2018, pp. 134–38. PubMed, https://doi.org/10.1016/j.clinre.2017.06.005.
Zhebrun, Daria, et al. “Association of PTPN22 1858T/T Genotype with Type 1 Diabetes, Graves’ Disease but Not with Rheumatoid Arthritis in Russian Population.” Aging (Albany NY), vol. 3, no. 4, Apr. 2011, pp. 368–73. PubMed Central, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3117451/.