Key takeaways:
~ Vitamin D plays an important role in your immune response, including helping fight off pathogens.
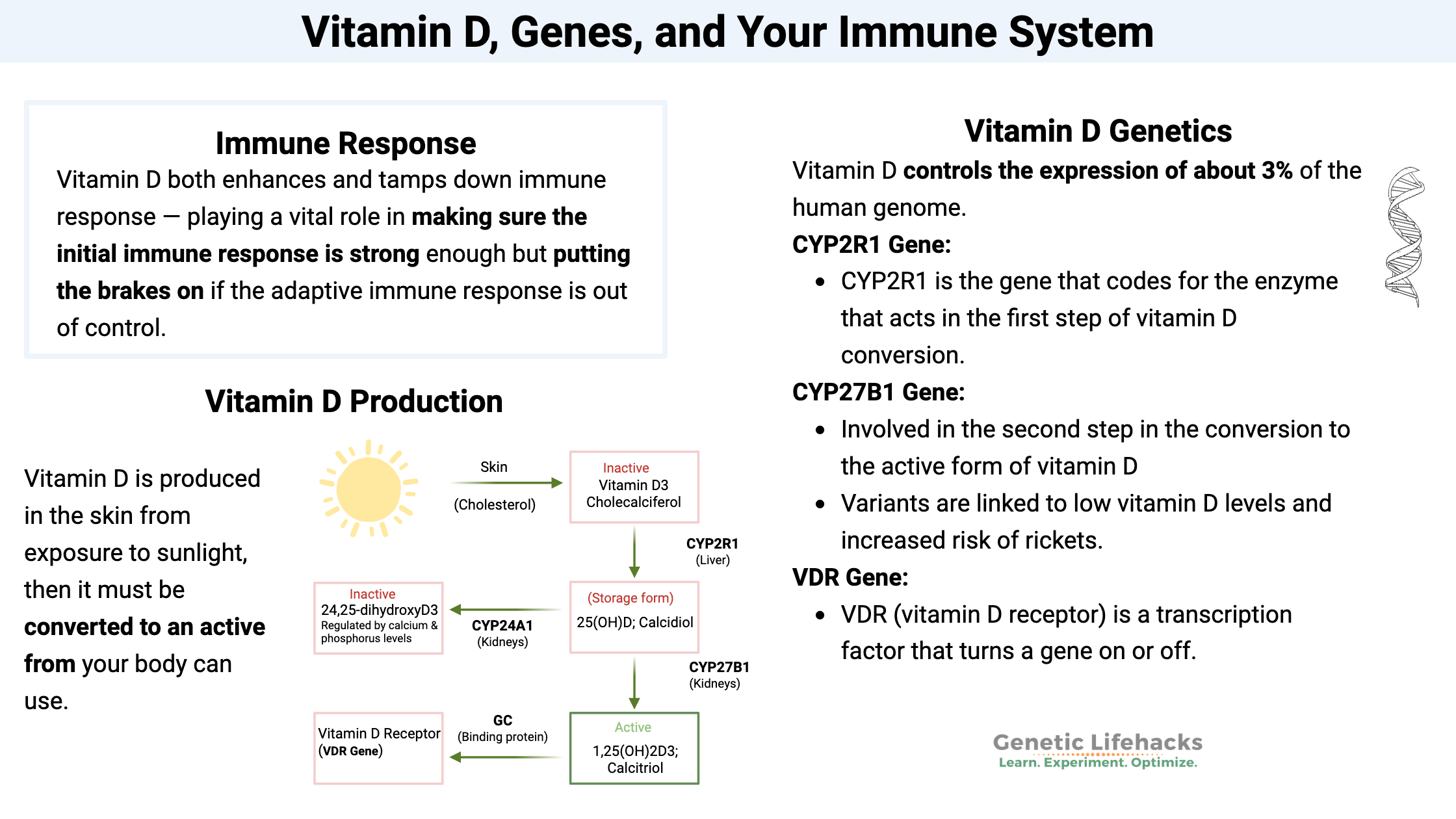
~ The body produces vitamin D through sunlight exposure and converts it into an active form through processes in the liver and kidneys.
~Vitamin D supplementation may benefit individuals with vitamin D deficiency, particularly in enhancing immune response and reducing the risk of respiratory infections. But its effects vary, and it is not a cure-all.
~ Genetic variants in the vitamin D genes can impact how likely you are to need supplemental vitamin D while also taking into consideration your sun exposure.
A Spanish randomized control trial recently showed that giving hospitalized COVID-19 patients vitamin D reduced the risk of an ICU stay by 98%![ref] This article explains how vitamin D interacts with the immune system and how to check your genetic data for vitamin D-related genes. We will wrap up with ways to increase your vitamin D levels.
Vitamin D and the Immune System:
Often, when you hear about vitamin D, it is in reference to strong bones and calcium regulation. But Vitamin D is also vital for your immune system – both in fighting off pathogens and in keeping your immune response in check so that it doesn’t get out of hand.[ref] Vitamin D is more than just a ‘vitamin’. It is actually a hormone that is essential to so many processes in your body, including your immune system.
Producing Vitamin D:
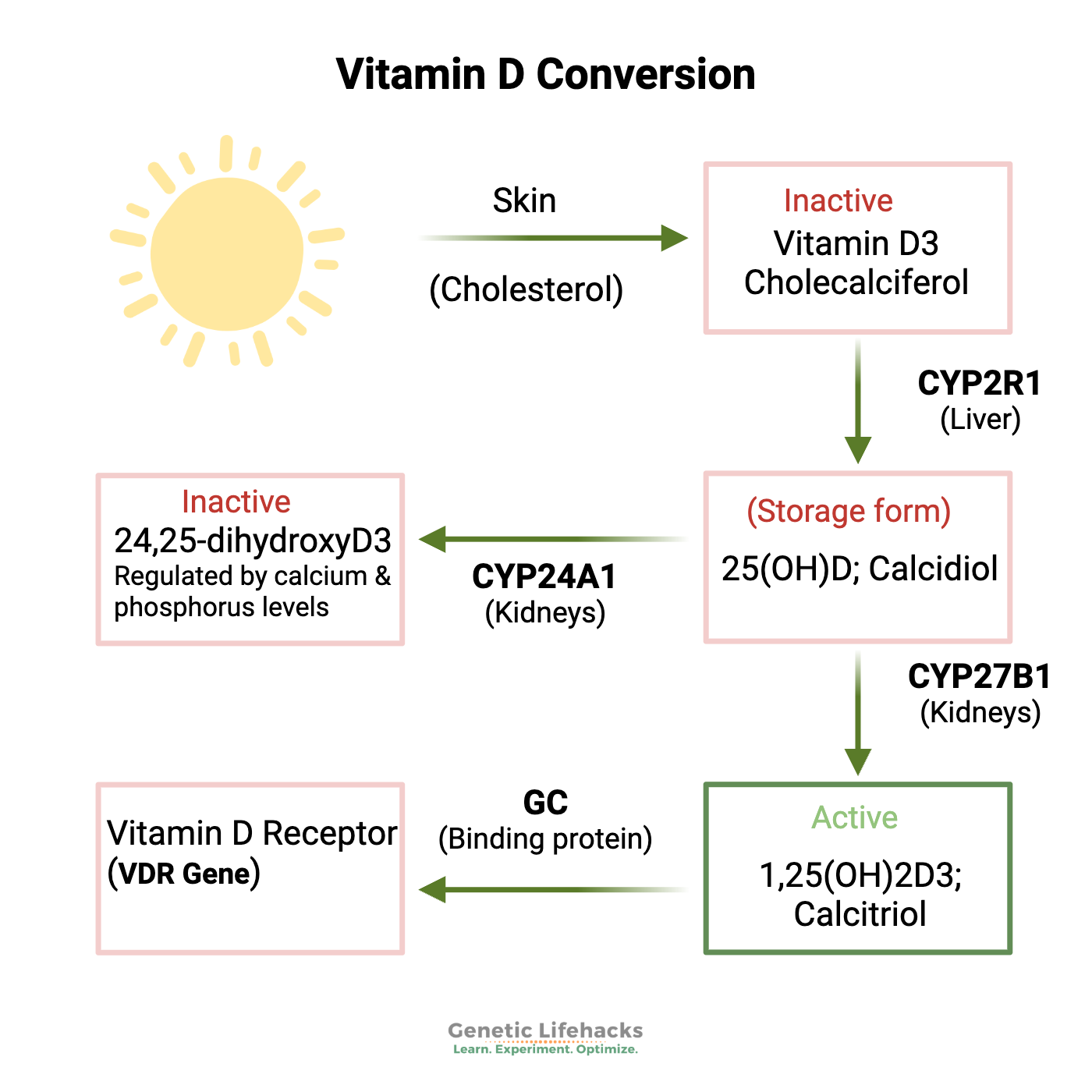
Vitamin D is produced in the skin from exposure to sunlight. It is produced via a reaction with UVB radiation and cholesterol in the skin.[ref] You can also get vitamin D through your diet.
Once your body makes D3 (cholecalciferol) or you absorb it from food, it goes through a couple of steps to convert it into an active form. First, it can be converted in the liver into 25-hydroxy vitamin D, or 25 (OH)D, with the help of an enzyme coded for by the CYP2R1 gene.
That 25(OH)D then needs to go through one more step to be the active form that your cells need. To convert the 25(OH)D into the active form – 1,25(OH)2D3 or calcitriol. The key enzyme for this conversion is coded for by the CYP27B1 gene.
Your body’s 25(OH)D levels are basically depending on how much you take in from food and sunlight. But the 1,25(OH)2D3 (calcitriol) levels are more tightly regulated, and the active form is converted when and where it is needed.
What exactly does vitamin D do?
In a nutshell, vitamin D can cause cells to turn on genes, making certain proteins needed in a cell.
To get a little more specific…
Inside your cells, vitamin D binds to the vitamin D receptor (VDR). This then causes VDR to get together with a couple of other proteins (one is a vitamin A-related receptor) and bind to different spots on the nuclear DNA. This activates the transcription of certain genes. In fact, vitamin D controls the expression of about 3% of the human genome. So, yeah, it’s pretty important.
Additionally, vitamin D can act as a hormone within cells to immediately cause non-DNA-related actions to take place, such as opening ion channels or causing the secretion of insulin.
The term pleiotropy gets used a lot in research papers about vitamin D. Pleiotropy just means that one gene (or in this case, one product of a gene, calcitriol) can cause more than one completely different action or trait to occur. In other words, vitamin D does a lot of stuff in the body that is seemingly unrelated. For example, vitamin D is essential for calcium regulation and strong bones — and vitamin D is also essential for immune response. It is also important in cancer prevention, hypertension, atrial fibrillation, blood clots, inflammatory bowel disease, and autoimmune disease.[ref]
A little history:
The Industrial Revolution in Northern Europe in the 1700s brought in crowded cities and thick air pollution from burning coal. Dirty skies and indoor jobs led to widespread rickets, a disease that causes bone deformation in children due to a lack of vitamin D. It is estimated that by the early 1900s, 80-90% of children had rickets in Northern Europe and the Northeast United States. This turned around in the 1930s when milk and other foods were being fortified with vitamin D, and the government was encouraging sun exposure for young kids.[ref] Baby cages became a popular way to put the kids out for some sun… (go look it up :-)
Immune response:
We can divide our body’s immune response into two parts:
- The innate immune response that happens immediately
- The adaptive response that develops to remember pathogens.
The innate response includes types of white blood cells known as monocytes and macrophages. You could imagine them as little Pac-Man coming in to gobble up the pathogens and cellular debris.
Macrophages contain both the vitamin D receptor (VDR) and CYP27B1, so they are able to use the circulating 25(OH)D to make the active calcitriol when needed. Macrophages use active vitamin D when initiated by interferon-gamma, which the innate immune system produces in response to pathogens such as viruses.[ref]
Interestingly, research shows that vitamin D both enhances and tamps down immune response — playing a vital role in making sure the initial immune response is strong enough but putting the brakes on if the adaptive immune response is out of control.[ref]
By the way, this knowledge of vitamin D helping immunity isn’t new! Healers have known for ages that sunlight is vital for health. Our great-grandparents probably reached for the cod liver oil, which is high in vitamin D, whenever the kids were sick. It was also used centuries ago as a primary treatment for tuberculosis (a lung disease caused by bacteria).
Vitamin D deficiency links obesity and immune response:
People who are obese are also more likely to be vitamin D deficient, and inflammation is a key linking factor here. In obesity, the fat cells can start giving off inflammatory signals and become infiltrated with macrophages.
Animal research clearly shows that low vitamin D levels increase inflammation significantly in obesity, and low vitamin D is also linked to increased fat mass. The research shows that low vitamin D levels cause the animals to burn less fat (lower fatty acid oxidation) and thus have more weight gain on a fattening diet. Additionally, inflammatory cytokines such as IL-6 and TNF-alpha are higher in mice fed an obesogenic diet that is low in vitamin D.[ref]
How is vitamin D deficiency defined?
Different countries and various research groups define vitamin D deficiency in varying ways.
- Severe vitamin D deficiency – less than 10 ng/mL – will cause rickets, which is a bone deformity disease.
- A lot of studies define vitamin D deficiency as <20 ng/mL, and the range between 20 -30 ng/mL is considered ‘insufficient’.
Basically, the statistically relevant bad effects of vitamin D tend to occur at levels of less than 30 ng/mL.[ref] Some groups recommend levels of 40-50 ng/mL as being optimal.
Studies on supplemental vitamin D and immune response:
There are a number of studies on vitamin D supplementation for viral and bacterial pathogens, and the outcomes range from no response to very positive effects.
- In patients with chronic hepatitis C (a viral disease), vitamin D deficiency (<30 ng/ml) is associated with more severe liver disease. A randomized control trial shows that correcting the deficiency helps to bring some of the inflammatory markers back into a good range, thus predicting better long-term outcomes for the patients.[ref]
- In HIV patients, vitamin D insufficiency (<30 ng/ml) and deficiency (<20 ng/ml) are associated with higher levels of inflammatory cytokines (IL-6, TNF-α, etc) and more activated monocytes.[ref]
- In kidney transplant patients, vitamin D deficiency is linked to an almost two-fold risk of urinary tract infections (bacterial).[ref]
- A meta-analysis of 18 studies on vitamin D and children found that low vitamin D is associated with an increased risk of acute lower respiratory infections (usually viral).[ref]
- A meta-analysis of a bunch of randomized, placebo-controlled trials in adults found that vitamin D supplementation reduced the risk of acute respiratory infections overall. The effect was mainly in those with low baseline vitamin D levels (<25 ng/mL).
- Supplemental vitamin D (1,200 IU and up) has been shown in several studies to be effective in decreasing the risk of influenza A (but not influenza B).[ref]
So does a vitamin D supplement cure everything? Well… probably not. There are quite a few studies showing that vitamin D supplements don’t do a lot for the population as a whole.
For example, a large 2019 study published in the New England Journal of Medicine showed that 2,000 IU of vitamin D/day did not affect cardiovascular disease outcomes, cancer rates, or all-cause mortality. The study was a clinical trial conducted in 25,000+ people, with half the group taking a placebo and half the supplemental vitamin D. It was a multi-ethnic study that followed participants for over 5 years.[ref]
On the other hand, a Cochrane analysis of 159 randomized trials concluded that vitamin D3 supplementation may be beneficial in older adults. It does show that vitamin D decreases the overall risk of cancer a little bit.[ref]
Instead of being a cure-all, my takeaway from reading through quite a few supplement studies is that vitamin D supplementation is important for the immune response in people who are vitamin D deficient. But for people with sufficient vitamin D levels, supplementation doesn’t show statistically significant benefits when looking at the population as a whole.
Vitamin D levels and SARS-CoV-2 susceptibility:
In the midst of the worldwide coronavirus outbreak, vitamin D has been in the spotlight. Numerous preprint articles since early on in the pandemic have noted that severe COVID-19 patients are much more likely to have vitamin D deficiency.[ref][ref][ref][ref]
There are a lot of mechanistic reasons why vitamin D deficiency would add to COVID-19 susceptibility. Top among these reasons is that vitamin D boosts the innate immune response (that initial response needed to kick the virus) and that vitamin D modulates the later immune overactivation, which causes acute respiratory distress syndrome.
A recent paper published in The Lancet explains:
“A role for vitamin D in the response to COVID-19 infection could be twofold. First, vitamin D supports production of antimicrobial peptides in the respiratory epithelium, thus making infection with the virus and development of COVID-19 symptoms less likely. Second, vitamin D might help to reduce the inflammatory response to infection with SARS-CoV-2. Deregulation of this response, especially of the renin-angiotensin system, is characteristic of COVID-19 and degree of overactivation is associated with poorer prognosis.”
Additionally, IL-6, which is a cytokine that causes much of the damage in severe COVID-19, is modulated by vitamin D.[ref]
A preprint analysis of the data in several vitamin D studies shows that about 90% of COVID-19 patients are either vitamin D deficient or insufficient. For this study, insufficiency was defined as being <20ng/mL.[ref]
A Chinese study found that vitamin D levels less than 30 nmol/L increased the risk of COVID severity by almost 3-fold.[ref]
Is it too late to boost your vitamin D levels once you have COVID? A randomized placebo-controlled study investigated the effects of 60,000 IU of oral vitamin D nano-liquid droplets daily for people who had mild SARS-CoV-2. The group receiving the vitamin D cleared the SARS-CoV-2 infection more quickly than the control group. Additionally, the vitamin D group also had a significant decrease in fibrinogen (clotting) levels.[ref]
A Spanish randomized control trial showed that giving hospitalized COVID patients vitamin D reduced the risk of ICU stays by 98%![ref]
Vitamin D Genotype Report:
Access this content:
An active subscription is required to access this content.
Related Articles and Topics:
Should you increase your vitamin C levels?
Like most nutrients, our genes play a role in how vitamin C is absorbed, transported, and used by the body. It can influence your risk for certain diseases, and it can make a difference in the minimum amount of vitamin C you need to consume each day.
Top 10 Genes to Check in Your Genetic Raw Data
Wondering what is actually important in your genetic data? These 10 genes have important variants with a big impact on health. Check your genes.
7 Genetic Variants That Increase Your Risk of Blood Clots
Genes matter when it comes to how quickly your blood clots – and whether you are at an increased risk for thrombosis. Learn about how blood clotting works and whether you are at risk.
References:
Ahn, Jiyoung, et al. “Genome-Wide Association Study of Circulating Vitamin D Levels.” Human Molecular Genetics, vol. 19, no. 13, July 2010, pp. 2739–45. PubMed Central, https://doi.org/10.1093/hmg/ddq155.
Atoum, Manar Fayiz, and Melya Nizar Tchoporyan. “Association between Circulating Vitamin D, the Taq1 Vitamin D Receptor Gene Polymorphism and Colorectal Cancer Risk among Jordanians.” Asian Pacific Journal of Cancer Prevention: APJCP, vol. 15, no. 17, 2014, pp. 7337–41. PubMed, https://doi.org/10.7314/apjcp.2014.15.17.7337.
Bjelakovic, Goran, et al. “Vitamin D Supplementation for Prevention of Mortality in Adults.” The Cochrane Database of Systematic Reviews, no. 1, Jan. 2014, p. CD007470. PubMed, https://doi.org/10.1002/14651858.CD007470.pub3.
Bouillon, Roger, et al. “Vitamin D and Human Health: Lessons from Vitamin D Receptor Null Mice.” Endocrine Reviews, vol. 29, no. 6, Oct. 2008, pp. 726–76. PubMed, https://doi.org/10.1210/er.2008-0004.
Chang, Eugene, and Yangha Kim. “Vitamin D Insufficiency Exacerbates Adipose Tissue Macrophage Infiltration and Decreases AMPK/SIRT1 Activity in Obese Rats.” Nutrients, vol. 9, no. 4, Mar. 2017, p. E338. PubMed, https://doi.org/10.3390/nu9040338.
Clifton-Bligh, Roderick J., et al. “Contribution of a Common Variant in the Promoter of the 1-α-Hydroxylase Gene (CYP27B1) to Fracture Risk in the Elderly.” Calcified Tissue International, vol. 88, no. 2, Feb. 2011, pp. 109–16. PubMed, https://doi.org/10.1007/s00223-010-9434-4.
—. “Contribution of a Common Variant in the Promoter of the 1-α-Hydroxylase Gene (CYP27B1) to Fracture Risk in the Elderly.” Calcified Tissue International, vol. 88, no. 2, Feb. 2011, pp. 109–16. PubMed, https://doi.org/10.1007/s00223-010-9434-4.
Davies, Gareth, et al. Evidence Supports a Causal Model for Vitamin D in COVID-19 Outcomes. 5 June 2020, p. 2020.05.01.20087965. medRxiv, https://www.medrxiv.org/content/10.1101/2020.05.01.20087965v2.
Entrenas Castillo, Marta, et al. “Effect of Calcifediol Treatment and Best Available Therapy versus Best Available Therapy on Intensive Care Unit Admission and Mortality among Patients Hospitalized for COVID-19: A Pilot Randomized Clinical Study.” The Journal of Steroid Biochemistry and Molecular Biology, vol. 203, Oct. 2020, p. 105751. PubMed, https://doi.org/10.1016/j.jsbmb.2020.105751.
—. “Effect of Calcifediol Treatment and Best Available Therapy versus Best Available Therapy on Intensive Care Unit Admission and Mortality among Patients Hospitalized for COVID-19: A Pilot Randomized Clinical Study.” The Journal of Steroid Biochemistry and Molecular Biology, vol. 203, Oct. 2020, p. 105751. PubMed, https://doi.org/10.1016/j.jsbmb.2020.105751.
Grant, William B., et al. “Evidence That Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths.” Nutrients, vol. 12, no. 4, Apr. 2020, p. 988. PubMed Central, https://doi.org/10.3390/nu12040988.
Hu, Zhiyong, et al. “The Association between Polymorphisms of Vitamin D Metabolic-Related Genes and Vitamin D3 Supplementation in Type 2 Diabetic Patients.” Journal of Diabetes Research, vol. 2019, Sept. 2019, p. 8289741. PubMed Central, https://doi.org/10.1155/2019/8289741.
Komolmit, Piyawat, et al. “Correction of Vitamin D Deficiency Facilitated Suppression of IP-10 and DPP IV Levels in Patients with Chronic Hepatitis C: A Randomised Double-Blinded, Placebo-Control Trial.” PLoS ONE, vol. 12, no. 4, Apr. 2017, p. e0174608. PubMed Central, https://doi.org/10.1371/journal.pone.0174608.
Kwon, Young Eun, et al. “Vitamin D Deficiency Is an Independent Risk Factor for Urinary Tract Infections After Renal Transplants.” Medicine, vol. 94, no. 9, Mar. 2015, p. e594. PubMed Central, https://doi.org/10.1097/MD.0000000000000594.
Larkin, Allison, and Jane Lassetter. “Vitamin D Deficiency and Acute Lower Respiratory Infections in Children Younger Than 5 Years: Identification and Treatment.” Journal of Pediatric Health Care, vol. 28, no. 6, 2014, pp. 572–82. PubMed Central, https://doi.org/10.1016/j.pedhc.2014.08.013.
Lau, Frank H., et al. Vitamin D Insufficiency Is Prevalent in Severe COVID-19. 28 Apr. 2020, p. 2020.04.24.20075838. medRxiv, https://www.medrxiv.org/content/10.1101/2020.04.24.20075838v1.
Luo, Xia, et al. “Vitamin D Deficiency Is Associated with COVID-19 Incidence and Disease Severity in Chinese People [Corrected].” The Journal of Nutrition, vol. 151, no. 1, Jan. 2021, pp. 98–103. PubMed, https://doi.org/10.1093/jn/nxaa332.
Manion, Maura, et al. “Vitamin D Deficiency Is Associated with IL-6 Levels and Monocyte Activation in HIV-Infected Persons.” PLoS ONE, vol. 12, no. 5, May 2017, p. e0175517. PubMed Central, https://doi.org/10.1371/journal.pone.0175517.
Manson, JoAnn E., et al. “Vitamin D Supplements and Prevention of Cancer and Cardiovascular Disease.” The New England Journal of Medicine, vol. 380, no. 1, Jan. 2019, pp. 33–44. PubMed, https://doi.org/10.1056/NEJMoa1809944.
McGrath, John J., et al. “A Systematic Review of the Association between Common Single Nucleotide Polymorphisms and 25-Hydroxyvitamin D Concentrations.” The Journal of Steroid Biochemistry and Molecular Biology, vol. 121, no. 1–2, July 2010, pp. 471–77. PubMed, https://doi.org/10.1016/j.jsbmb.2010.03.073.
Petersen, Rikke A., et al. “Common Genetic Variants Are Associated with Lower Serum 25-Hydroxyvitamin D Concentrations across the Year among Children at Northern Latitudes.” The British Journal of Nutrition, vol. 117, no. 6, Mar. 2017, pp. 829–38. PubMed, https://doi.org/10.1017/S0007114517000538.
Rastogi, Ashu, et al. “Short Term, High-Dose Vitamin D Supplementation for COVID-19 Disease: A Randomised, Placebo-Controlled, Study (SHADE Study).” Postgraduate Medical Journal, Nov. 2020, p. postgradmedj-2020-139065. PubMed, https://doi.org/10.1136/postgradmedj-2020-139065.
—. “Short Term, High-Dose Vitamin D Supplementation for COVID-19 Disease: A Randomised, Placebo-Controlled, Study (SHADE Study).” Postgraduate Medical Journal, Nov. 2020, p. postgradmedj-2020-139065. PubMed, https://doi.org/10.1136/postgradmedj-2020-139065.
Rhodes, Jonathan M., et al. “Editorial: Low Population Mortality from COVID-19 in Countries South of Latitude 35 Degrees North Supports Vitamin D as a Factor Determining Severity.” Alimentary Pharmacology & Therapeutics, vol. 51, no. 12, 2020, pp. 1434–37. Wiley Online Library, https://doi.org/10.1111/apt.15777.
Smet, D. De, et al. Vitamin D Deficiency as Risk Factor for Severe COVID-19: A Convergence of Two Pandemics. 19 May 2020, p. 2020.05.01.20079376. medRxiv, https://www.medrxiv.org/content/10.1101/2020.05.01.20079376v2.
Trochoutsou, Aikaterini I., et al. “Vitamin-D in the Immune System: Genomic and Non-Genomic Actions.” Mini Reviews in Medicinal Chemistry, vol. 15, no. 11, 2015, pp. 953–63. PubMed, https://doi.org/10.2174/1389557515666150519110830.
—. “Vitamin-D in the Immune System: Genomic and Non-Genomic Actions.” Mini Reviews in Medicinal Chemistry, vol. 15, no. 11, 2015, pp. 953–63. PubMed, https://doi.org/10.2174/1389557515666150519110830.
Vanherwegen, An-Sofie, et al. “Regulation of Immune Function by Vitamin D and Its Use in Diseases of Immunity.” Endocrinology and Metabolism Clinics of North America, vol. 46, no. 4, Dec. 2017, pp. 1061–94. PubMed, https://doi.org/10.1016/j.ecl.2017.07.010.
VCV000001661.1 – ClinVar – NCBI. https://www.ncbi.nlm.nih.gov/clinvar/variation/1661/. Accessed 14 Dec. 2021.
Wacker, Matthias, and Michael F. Holick. “Sunlight and Vitamin D.” Dermato-Endocrinology, vol. 5, no. 1, Jan. 2013, pp. 51–108. PubMed Central, https://doi.org/10.4161/derm.24494.
Wu, Yingying, et al. “Polymorphisms of CYP27B1 Are Associated with IFN Efficacy in HBeAg-Positive Patients.” Journal of Clinical Laboratory Analysis, vol. 32, no. 5, June 2018, p. e22367. PubMed, https://doi.org/10.1002/jcla.22367.
Xu, Xun, and Minghao Shen. “Associations between Vitamin D Receptor Genetic Variants and Tuberculosis: A Meta-Analysis.” Innate Immunity, vol. 25, no. 5, July 2019, pp. 305–13. PubMed, https://doi.org/10.1177/1753425919842643.
Yu, Songcheng, et al. “Family-Based Association between Allele T of Rs4646536 in CYP27B1 and Vitamin D Deficiency.” Journal of Clinical Laboratory Analysis, vol. 33, no. 6, July 2019, p. e22898. PubMed, https://doi.org/10.1002/jcla.22898.
Zisi, Dimitra, et al. “The Association between Vitamin D Status and Infectious Diseases of the Respiratory System in Infancy and Childhood.” Hormones (Athens, Greece), vol. 18, no. 4, 2019, pp. 353–63. PubMed Central, https://doi.org/10.1007/s42000-019-00155-z.
—. “The Association between Vitamin D Status and Infectious Diseases of the Respiratory System in Infancy and Childhood.” Hormones (Athens, Greece), vol. 18, no. 4, 2019, pp. 353–63. PubMed Central, https://doi.org/10.1007/s42000-019-00155-z.
—. “The Association between Vitamin D Status and Infectious Diseases of the Respiratory System in Infancy and Childhood.” Hormones (Athens, Greece), vol. 18, no. 4, 2019, pp. 353–63. PubMed Central, https://doi.org/10.1007/s42000-019-00155-z.
Debbie Moon is a biologist, engineer, author, and the founder of Genetic Lifehacks where she has helped thousands of members understand how to apply genetics to their diet, lifestyle, and health decisions. With more than 10 years of experience translating complex genetic research into practical health strategies, Debbie holds a BS in engineering from Colorado School of Mines and an MSc in biological sciences from Clemson University. She combines an engineering mindset with a biological systems approach to explain how genetic differences impact your optimal health.