The news headlines can be confusing. The talking heads on TV seem to change their minds daily. And Google search results can be contradictory!

So let’s cut through the BS and look at the research studies on vitamin D and SARS-CoV-2 (and genetics, of course).
Related article: Research roundup: Preventing and Mitigating Covid-19
Why is vitamin D important for the immune system?
Vitamin D is a hormone produced in the skin upon UV exposure. The precursor molecule for vitamin D is cholesterol.
Once produced, vitamin D is stored in an inactive form and then activated when needed. Many of the actions of vitamin D in the body are a result of its binding to a vitamin D receptor. This results in eventually turning on or off other genes for transcription.
When active vitamin D binds to its receptor (VDR), the molecule can enter the nucleus of the cell and bind to vitamin D responsive elements on the DNA, resulting in gene transcription. Targets of VDR include genes important in bone health, cardiovascular health, and the immune system.
What does this have to do with our immune system?
A type of white blood cell called a macrophage contains both the vitamin D receptor (VDR) and the ability to turn the circulating inactive form of vitamin D into the active form when needed. Macrophages use active vitamin D when initiated by interferon-gamma, which the innate immune system produces in response to pathogens such as viruses.[ref] This active vitamin D combines with the VDR to then activate several genes needed in the fight against viruses.
Interestingly, research shows that vitamin D both enhances and tamps down the immune response — playing a vital role in making sure the initial immune response is strong enough…But then putting the brakes on if the adaptive immune response is out of control.[ref]
Can Vitamin D help to protect against COVID?
Early on in the pandemic, published research studies suggested that people with low vitamin D levels were much more likely to have severe cases of COVID-19 and were at a greater risk of dying.[ref]
But those studies were observational and left a lot of questions unanswered. Questions such as ‘were the people with low vitamin D already sick and likely to die of any infection?’. A chronic or extended illness can cause vitamin D deficiency…
Over the past year and a half, many studies have tried to determine if vitamin D supplementation can protect against getting COVID-19.
Let’s take a look at the studies:
In Korea, a study of COVID-19 patients found that they had sufficient vitamin B1, B6, B9, B12, and zinc levels. The one deficiency found was severe vitamin D deficiency.[ref]
A study of elderly SARS-CoV-2 patients found that they had significantly lower vitamin D levels than an age-matched control group.[ref]
In the United Arab Emirates, researchers found that low vitamin D levels were associated with severe COVID-19. The study concluded:[ref]
Levels < 12 ng/mL were significantly associated with higher risk of severe COVID-19 infection and of death. Age was the only other independent risk factor, whereas comorbidities and smoking did not contribute to the outcomes upon adjustment.
A July 2021 study showed that 84% of patients with COVID-19 (n=191) had vitamin D deficiency or insufficiency. This was a stark contrast to their age-matched healthy control group, in which only 32% of people had insufficient vitamin D levels. [ref]
Not all studies reported a connection between vitamin D levels and outcomes. A study in Nature concluded that patients with vitamin D deficiency were at no greater risk of severe COVID than the group without vitamin D deficiency.[ref] Oddly, though, the vitamin D deficient group was 11 years younger than the other arm of the study. Thus, a different conclusion would be that vitamin D deficiency in your mid-40s is equivalent to the risk of being in your late 50s…
Summing it up:
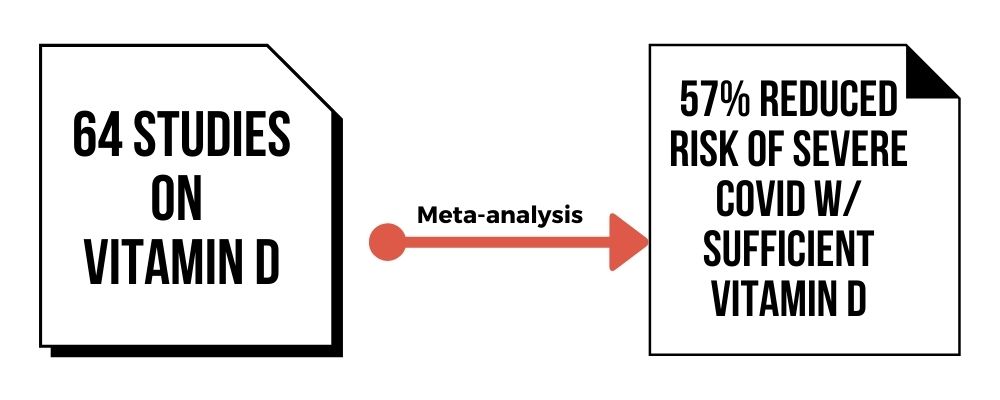
A meta-analysis of 64 studies on vitamin D sufficiency and COVID-19 prevention shows that having adequate vitamin D reduced the risk of severe COVID by 57% (as of Aug. 10, 2021).[ref]
Is ‘more’ always better?
The research studies on vitamin D show that not being deficient is likely enough to help with your immune system response to COVID-19.
More is not always better, and in this case, having an adequate level seems to be good enough. Most studies put an adequate vitamin D level at anything over 30 ng/ml, but a couple of studies use 50 ng/ml.
That said – vitamin D deficiency is widespread. You need to do a blood test to figure out your actual vitamin D level.
Can vitamin D help once you have covid?
You may be wondering if vitamin D does anything if you are already sick. The research on this seems to point to high-dose vitamin D being helpful early on in severe cases, but by the time the patient reaches the ICU, it may be too late.
Here’s what the research says:
A small trial found that vitamin D, B12, and magnesium before getting COVID-19 helped to protect against needing oxygen or intensive care support.[ref]
Another small randomized control trial found that high-dose supplemental vitamin D upon being admitted to the hospital decreased the risk of ICU admittance by 98%. Keep in mind that it was a small trial (75 patients) so that percentage is likely skewed.[ref]
A randomized clinical trial in people with mild to moderate COVID showed that 5,000 IU daily of vitamin D reduced the time that they were sick.[ref] Note that the study was done in people who had ‘sub-optimal’ vitamin D levels and that the control group took 1,000 IU of vitamin D daily.
In Spain, hospitalized COVID-19 patients who received vitamin D supplements daily were at an 84% decreased risk of death.[ref]
Not all studies show a positive outcome, though.
A Brazilian study found that a single, high-dose vitamin D shot did not significantly reduce hospital length of stay.[ref] Other studies also show little effect from vitamin D given to patients in the ICU.[ref]
Thus, vitamin D supplements may depend on timing, and there is likely a point after which vitamin D doesn’t help.
Should you take vitamin D before getting ‘the jab’?
This is a question that is harder to answer since vitamin D has a moderating effect on some immune functions.
Research on vitamin D supplementation before the flu shot showed that it promoted a higher TGF-beta plasma level but that it didn’t affect antibody production.[ref] If this is the same for the mRNA vaccines, then it may not matter if you take vitamin D before getting a COVID vaccine.
The CDC is silent on this topic. They do recommend that you abstain from ibuprofen or acetaminophen before getting the vaccine.[ref]
How do vitamin D genes impact COVID-19 risk?
You may be wondering – what if my vitamin D genes are ‘bad’? Could that cause COVID?
Quick answer: Probably not.
Related article: Vitamin D genes and your immune system
One way that researchers determine how genes influence an outcome is through genome-wide association studies (GWAS). These types of studies use a huge amount of genetic data from tens of thousands of study participants to see if there is a statistical increase in the likelihood of an outcome due to a genetic variant.
Genome-wide association studies on COVID-19 patients have found that genetic variants in immune system genes and coagulation factor genes slightly increase (or decrease) the risk of getting severe COVID-19.[ref][ref] GWAS studies did not consider vitamin D genes as a risk factor.
Another way that researchers probe genetic connections to a disease is through a Mendelian Randomization study. This is kind of the opposite of a GWAS study. The researchers use known genetic variations to see if those variants interact with environmental factors in causing disease. For example, Mendelian randomization studies show that genes that increase LDL cholesterol are linked to heart disease — thus taking away the conflicting factors of a diet high in saturated fat.
A recent Mendelian randomization study also did not show that genetic variants associated with higher vitamin D levels are protective against COVID-19.[ref]
Lifehacks:
There is a clear signal that low vitamin D levels increase susceptibility to COVID-19. It isn’t entirely clear how much -or if- you should supplement with vitamin D to prevent COVID. But the research is clear that being deficient in vitamin D increases the risk of a lot of diseases — and there is little or no downside to getting your vitamin D levels into the normal range.
Sun exposure on your skin during the middle hours of the day is a great way to maintain your vitamin D levels. But this can be difficult if you work inside all day or during the winter months.
A UK study in 2007 showed that, on average, vitamin D levels dropped by half in the winter and spring compared to summer and fall.[ref]
This drop in vitamin D isn’t instantaneous, though. Your fat cells can store the inactive form of vitamin D, so even though sun exposure drops by September, you may still have some reserve vitamin D for a couple of months.[ref]
Common sense advice:
If you are deficient in vitamin D (test to find out), then consider supplementing with a good quality vitamin D supplement. Read the ingredients. It’s my preference to take vitamin D in capsule form that contains good fat, like coconut oil. If you wouldn’t normally consume cottonseed oil or soybean oil, don’t take vitamin D encapsulated with it. If you are taking a vitamin D pill that doesn’t include fat, be sure to take it with a meal that contains some fat.
Vitamin D is a supplement that is safe for almost everyone to take. If you have a rare condition that prevents you from supplementing, go with your doctor’s advice. For the rest of us, there are few drawbacks to supplementing with an inexpensive vitamin when needed.
We all need to take a look at our lifestyle and health issues to try to prevent the spread of all respiratory diseases. No treatment at this point seems to be 100% effective at preventing the viral infection. Having a sufficient vitamin D level is one tool in the prevention of (severe) COVID-19 and an easy one to do.
Relates Articles and Topics:
COVID-19 & Genetics: Who gets sick and why?
Genetic variants play a role in susceptibility to infectious diseases. Not everyone will get the norovirus or a particular strain of the flu — due to genetic variants. New research shows that genetics also plays a role in the severity of COVID-19.
Genetic risk and Guillain-Barré syndrome
Our immune system is amazingly powerful, protecting us against known and unknown foreign invaders. Occasionally, things go awry, and autoimmune diseases, such as Guillain-Barré syndrome, can occur.
Acute Respiratory Distress Syndrome Genes
This is article explains what happens to the body in ARDS, and it goes into the genetic variants that increase or decrease the risk of ARDS (due to all causes – not just COVID-19). ARDS is a ‘syndrome’, and thus a collection of symptoms rather than a disease.